
Laboratory techniques that make genetic profiling and mutation monitoring of tumours more readily accessible than by direct tissue biopsy have recently been introduced. These techniques, based on the detection of circulating tumour DNA (ctDNA), have become known as liquid biopsies because they rely on peripheral blood sampling, write Bruno Damascelli, Vladimira Tichà, Elena Repetti and Tshering Dorji, Milan, Italy.
Detection of somatic mutations in circulating DNA is comparable to that obtained from tumour tissue biopsy, but with a direct therapeutic advantage in that the molecular diagnosis can be updated through noninvasive serial sampling. Liquid biopsy also includes detection of circulating tumour cells (CTCs) that can be characterised by immunofluorescence, contributing to a precise molecular diagnosis.
The number of CTCs is small and a peripheral blood sample may contain only one tumour cell for every 600,000 nucleated cells. Likewise, fragmented DNA derived from tumours is found only in small amounts, mixed with DNA resulting from normal cell death, which accounts for at least 90%. Despite these limitations, liquid biopsy is gaining ground and has been internationally validated for non-small-cell lung cancer, melanoma and colorectal cancer.
Laboratory methods are improving daily and target sequencing and target mutation techniques are becoming increasingly effective in detecting a larger number of mutations and identifying single mutations of direct interest for targeted molecular therapy.
In just the same way as selective sampling is used for localisation of hormone-producing tumours, we decided to use selective venous catheterisation to overcome, in part, the dilution effect that ctDNA and CTCs undergo in peripheral blood. The circulation draining any part of the body can be reached by percutaneous venous mini-catheterisation via brachial, jugular or femoral puncture, according to standard interventional radiology practice. There are no contraindications to the procedure, which is carried out in an outpatient setting with acceptable invasiveness and can be repeated any number of times.

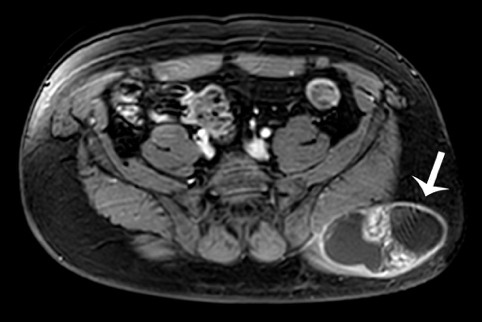
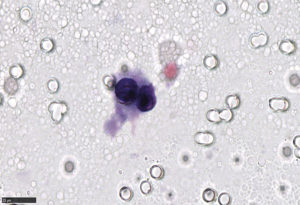
In a preliminary clinical series, liquid biopsy carried out in parallel on selective and peripheral blood samples yielded interesting results. In the case of sarcoma of the left gluteus shown by way of example, target sequencing on a peripheral blood sample and on a selective sample from the left hypogastric artery showed a TP53 gene mutation, which can indicate tumour sensitivity to treatment with doxorubicin and ifosfamide. A tumour cell cluster was detected only in the selective sample (Figures 1–3).
Bruno Damascelli and Vladimira Tichà are with EmoGVM Centrocuore Columbus, Milan, Italy. Elena Repetti is with IMPACTLAB, Department of Genetics, Milan, Italy, and Tshering Dorji is with LAMM – IMPACTLAB Group, Department of Pathology, Milan, Italy. None of the authors reported any disclosures pertaining to this article.













