Speaking at the 32nd Annual International Symposium on Endovascular Therapy (ISET; 22–25 January, Hollywood, USA), Lindsay Machan (University of British Columbia, Vancouver, Canada) said that there had been “significant advancements” in the development of radiation protection options, though added that it was “important to remember that all devices are tested in optimised, non-real world conditions”.
“We are all aware of some very inconvenient truths about radiation,” he began, highlighting how, in 2017, “It was pointed out that in all these procedures we are performing, not only do they cause evidence of radiation-induced DNA damage, but we are individually predisposed, and actually the less radiation we get exposed [to], the less DNA damage we get from doing those procedures.”
Of the multitude of new procedures for radiation protection that have emerged in the last few years, Machan said he believes they could be categorised into three general brackets. These are: protective shielding, reducing the radiation output, and reducing the biological effect.
Protective shielding
“I think most of us are used to the idea of using shielding,” Machan said. “If you use the new three metal shielding [triple layer non-lead skirts], it actually works profoundly well.” He showed the ISET audience a video of physicians performing an endovascular aneurysm repair (EVAR), commenting that his own data show that if, in addition to the “typical shielding and the bedside shielding”, a triple layer non-lead skirt was added to the theatre set-up, “you can actually reduce radiation to the operator by 91% compared to what we call ‘commando’, or just wearing a lead [apron]”.
Adding more additional shielding resulted in a further 80% reduction in radiation exposure to the operator and staff, Machan shared. He showed the ISET audience “some pretty innovative lead gowns”, again with the tripe metal layering. The gowns are made from tungsten, antimony, and bismuth, the “secret sauce”, in Machan’s words. Speaking of this metal triplet, he said he “highly encouraged” his listeners to look into acquiring such a combination gown for their own practice.
“It is actually very light,” he said of the gown. “Compared to standard non-lead, so called ‘light’ lead, this is profoundly better in terms of radiation protection,” he emphasised. For a 0.25mm thick gown, the wearer would get 3.7% transmission from a 70kV beam, Machan said. In contrast, this drops to 1.7% transmission with a 0.35mm thick gown, and reduces further to 0.6% transmission with the triple metal gown, which is 0.5mm thick.
However, he also offered a word of caution. When investigating the radiation protection conferred by lead glasses, Machan reported that they were not particularly effective. Describing their experimentation, Machan said: “The magic innovation was eyelash glue that allowed us to put dosimeters on the face—the eyelids and the cheeks. We then put lead glasses over the top, and it was a little bit disturbing to find that in real-world circulations, lead glasses only reduce the radiation dose to the eye by 9.5%. If you look at the right eye, it is 14.2%, so in other words, our nose actually provides 15% of radiation protection. These things are tested in non-real-world circumstances; this needs our attention.”
Reducing the radiation output
In terms of reducing the radiation output, Machan said he was “conflicted”.
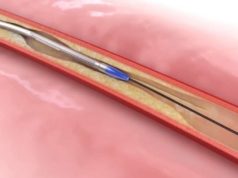
“There are many different ways of doing this, he stated. One way utilises artificial intelligence (AI) to limit the radiation exposure when using fluoroscopy to navigate intraprocedurally. “When we are doing procedures,” Machan explained, “we are usually focusing on a relatively small area of the image [generated by fluoroscopy]. We have used AI, and we have taught it to recognise catheters, guidewires, and contrast, and then we use that to guide sub-second coning to our areas of interest. Once per second, we open up the full field, so you get context.
“You step on the fluoro-pedal, and where the white box is [a white box is visible over a subsection of the fluoroscopy image], that is the AI actually changing the cones actively. It just looks like normal fluoroscopy.”
The first application of AI-enabled fluoroscopy demonstrated that it facilitated a median 61.8% radiation dose reduction to the patient, and a 59.4% reduction to everybody else in the operating theatre.
Reducing the biological effect
“This is interesting work reducing the biological effect of radiation,” Machan said, introducing work by Kieran Murphy (University Health Network Toronto Western Hospital, Toronto, Canada).
Explaining this research, Machan recounted: “All of us sitting here, we have this balance of excess free radicals and anti-oxidants to prevent DNA damage and oxidative stress. Radiation creates free radicals, which damage DNA, and results in all those noxious things that we talk about: stroke, heart attack, cancer, cataracts, and accelerated aging. Kieran [Murphy]’s thought is that if you take an anti-oxidant mixture dissolved in any drink, even ones we do not think of as being healthy, and if you do this every day before you go in and do a procedure, then actually the idea is that you prevent those free radicals from damaging your DNA.”
In a clinical study of 10 patients published in the Journal of Vascular and interventional Radiology (JVIR) in 2017 by Murphy et al, the investigators found that premedication with an oral antioxidant cocktail before medical imaging exams could significantly reduce DNA injury from the ionising radiation dose. Murphy claimed at ISET that this was “pretty impressive early phase work”, and teased that Murphy’s group were preparing to do the same kind of study on people before they do endovascular procedures.
However, whilst Machan is enthusiastic about these various options for radiation protection, eh concludes by saying that “There is no safe dose”.