Premedication with an oral antioxidant cocktail before medical imaging exams could significantly reduce deoxyribonucleic acid (DNA) injury from the ionising radiation dose, finds new research presented at the Society of Interventional Radiology’s annual scientific meeting in Atlanta, USA.
“An oral antioxidant cocktail of seven pills including beta-carotene, vitamin C, alpha lipoic acid and n-acetyl cysteine offered prior to medical imaging for screening or intervention, may result in a reduction in cancer induction risk. Our results suggest that antioxidant pre-medication can protect DNA from damage induced by X-rays in medical imaging exams. The implications for cancer induction are speculative,” said Kieran Murphy, University Health Network Toronto Western Hospital, Toronto, Canada, who was presented the 2015 SIR Foundation Leaders in Innovation Award.
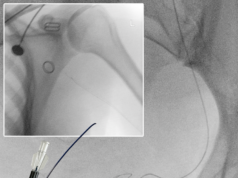
Murphy highlighted that the volume of medical imaging exams is constantly increasing with patients being exposed to ionising radiation every day, particularly in the context of computed tomography, X-ray and fluoroscopy. The exposure occurs in radiology departments, but also in the operating room, cardiac catheterisation labs, etc. “Diagnostic imaging examinations, computed tomography and fluoroscopy in particular, are associated with radiation doses generally ranging between 0.02 and 40mSv2 and may cause malignant transformation of patient’s cells and tissues which, many years later, manifest as cancer or posterior chamber cataracts. Cancer risk from medical imaging exams is a function of age. Patients who are particularly at risk include those undergoing complex cardiac PET CT, chemotherapy, gallium scans, MRI radiofrequency coils and high fields. Interventional radiologists should also consider the risks they expose themselves to on a daily basis,” he noted.
Murphy explained that the mutagenic effect of ionising radiation is clearly established through a variety of molecular mechanisms including double stranded DNA breaks, single DNA strand breaks, nucleotide substitution and sugar/ribose alterations.
“A cell responds to focal DNA damage through initiation of a biochemical repair mechanism constituting a protein complex being bound to the DNA strand at the defect. Every cell has a DNA repair apparatus. This is a protein complex that fixes DNA lesions before the cell replicates, without this apparatus, we would all get cancer. The mechanism is a complex of repair proteins, one of which is gamma-H2AX,” Murphy explained.
Whilst there are several major biochemical tests to quantify DNA damage, the most sensitive involves quantifying DNA damage with 3D microscopy using fluorescently labeled gamma-H2AX protein.
“Our initial work focused on in vitro antioxidant premedication. In these cases we would pipette antioxidants into blood tubes prior to their irradiation to test a treatment effect. We also measured reduction in DNA injury as a function of antioxidant dose. Initially we used high radiation doses (~2Gy) to best demonstrate an effect. Then we proceeded to lower doses more typical of diagnostic exams. We saw a substantial reduction in DNA injury as a result of antioxidant premedication and so began to study the ability of antioxidant chemicals to decrease the genetic damage associated with CT examinations,” he noted.
The researchers performed a prospective randomised study in 10 patients undergoing technetium methylene diphosphonate bone scans with identical doses. Patients were randomised to premedication (5) or no premedication (5). The patients were given a set of oral antioxidants one hour before they were scheduled to receive a bone scan.
“Premedication with our current formulation of antioxidants significantly reduced formation of gamma-H2AX and 53BP1 foci after injection of a clinically standard radiation dose of technetium for a bone scanning. Based on this experience, 60 minutes prior to Tracer injection was adequate to achieve a 90% reduction in foci,” Murphy noted.
In the control bone scan patients, the gamma-H2AX foci in lymphocytes post radiation were significantly higher than seen pre-radiation, suggesting that there had been significant DNA damage and subsequent repair initiated. On the other hand, in the bone scan patients who received the antioxidant treatment, the gamma-H2AX foci in the lymphocytes were not significantly raised after radiation, suggesting that there had been less radiation damage.