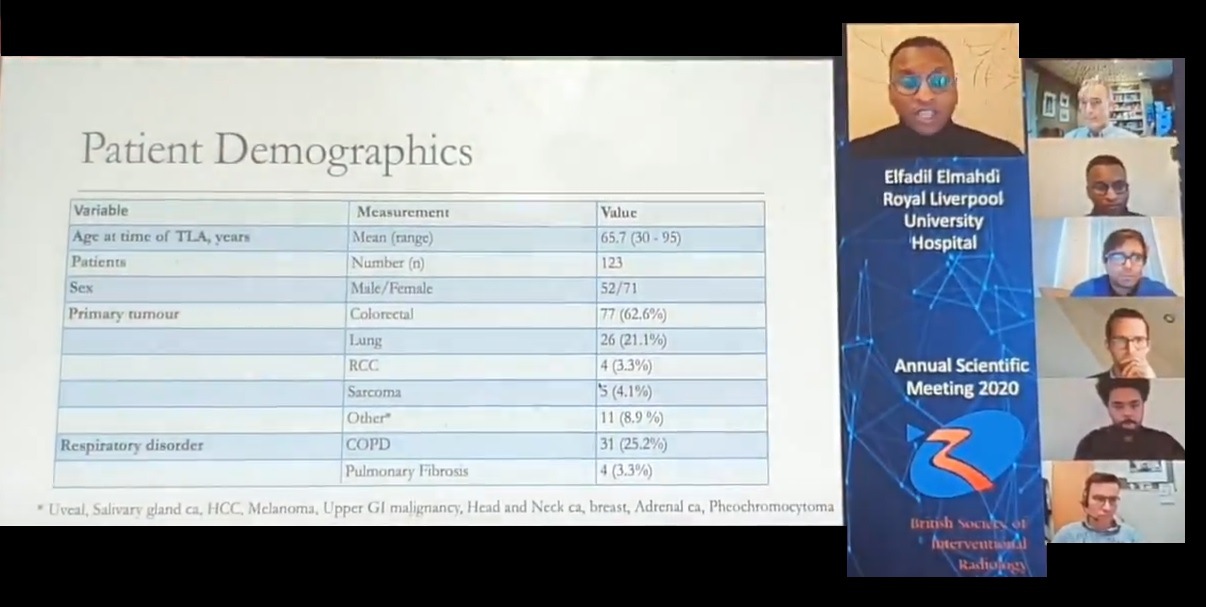
Thermal lung ablation (TLA) is an effective treatment, resulting in good overall survival with good local control, attendees were told at the 2020 annual scientific meeting of the British Society of Interventional Radiology (BSIR; 1–3 December, online). Elfadil Elmahdi (Royal Liverpool University Hospital, Liverpool, UK) presented his ten-year experience of the non-invasive alternative to surgical resection at a tertiary hospital.
Elfadil and colleagues conducted a retrospective, observational review to evaluate local tumour control, overall survival, and complications of TLA in their centre between 2009 and 2019. While 128 patients in total were treated with TLA during this period, five were excluded from the study for disease progression prior to TLA and no follow-up data. Between the 123 patients analysed in the study, 321 nodules were ablated.
Technical success was achieved in 301 nodules (93.8%). Of the 20 unsuccessful procedures, 14 nodules underwent a repeat ablation.
Showing a Kaplan-Meier graph depicting local recurrence, Elfadil informed his audience that the mean number of years before local recurrence was 10.5 years (±0.234; confidence interval [CI]: 10.07–10.99), with one-, two-, and three-year survival without local recurrence being 90%, 87.5%, and 86%, respectively. A second Kaplan-Meier graph, this time depicting new pulmonary recurrence, showed that the mean time before new tumours developed again was 5.8 years (±0.414; CI: 4.95–6.57), with the one-, two-, and three-year survival rate with no new pulmonary occurrence being 85%, 72%, and 60%, respectively.
Median overall survival was 3.16 years (±0.305; CI: 2.56–3.76). One-, two-, and three-year overall survival was 98%, 82%, and 56%, respectively. These survival rates are comparable to other TLA studies, Elfadil said, “if not slightly better”.
A pneumothorax requiring a chest drain was seen in 50.7% of patients—again, Elfadil told delegates that this was similar to that reported in the literature.
Addressing the limitations of the presented study, he went on to say that the investigators assumed that TLA practice in the Royal Liverpool University Hospital was homogenous between operators over time, co-morbidities that may influence survival were not taken into account, and no correlation was made with the grades of the primary tumour. In addition, there are reservations to what can be achieved with a retrospective study design using data from a single institution. lung ablation