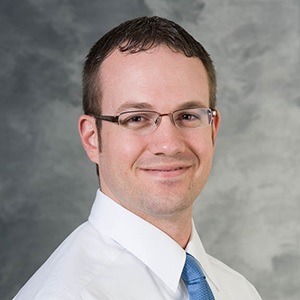
Preliminary results of a first in man trial demonstrate that robotically-assisted sonic therapy (RAST) can create a planned ablation volume without significant device-related adverse events. Timothy Ziemlewicz (Department of Radiology, University of Wisconsin School of Medicine and Public Health, Madison, USA) informed delegates at the 2019 annual meeting of the Society of Interventional Oncology (SIO; 7–11 June, Boston, USA) that short-term local tumour control with RAST may be similar to that of other ablation modalities.
The study investigators conducted a phase I trial with the aim of evaluating the safety and short-term efficacy of RAST for hepatic ablation in patients with primary or metastatic liver cancer. RAST is the automated treatment of a defined volume of tissue utilising histotripsy, the first non-thermal, non-ionizing, non-invasive ablation modality. Prior to this research, RAST had successfully been applied in pre-clinical porcine liver models.
The study patients were recruited from, and procedures were performed at, two hospitals near Barcelona, Spain: Mutua Terrassa, where the study’s principal investigator Joan Vidal-Jove is located, and Vall D’Hebron Hospital, where Xavier Serres is based. The underlying technology was developed by members of the Department of Biomedical Engineering at the University of Michigan.
When delineating the advantages of RAST, Ziemlewicz emphasised the precision, telling the SIO audience that the cavitation bubble cloud is precise at the histologic level (“so you can literally cut cells in half with it”), and that planned treatment volumes are within nanometres of the resultant ablation.
The phase I, open-label, non-randomised trial had a primary endpoint of technical success, defined as the ability to create an ablation zone per the planned volume, as assessed by MRI one-day post-procedure. There were multiple secondary endpoints, the most important of which, according to Ziemlewicz, was safety, measured as the number and severity of adverse events. Adverse events were graded using the Common Terminology Criteria for Adverse Events (CTCAE v4.0), a descriptive scale from Grade 1 (mild) through to Grade 5 (death related to adverse event). The study investigators also evaluated local tumour progression, liver function, involution of the ablation zone, and analgesic requirements. Follow-up MRI, laboratory draws, and clinical visit were planned at one day, one week, one month, and two months.
Eight patients, five female, three male, have had a tumour treated under this protocol. Most patients (six) had a single tumour, one patient had two tumours, and one patient had three tumours. The mean tumour size was 1.3cm, and the range was 0.5cm to 2.3cm. “We were somewhat limited in size by having to fit treatments within livers with multifocal tumours”, Ziemlewicz said.
The triallists achieved 100% technical success in creating the planned ablation volume using RAST. In the axial plane, the ablation zone was within an average of 0.1cm of the plan, and in the coronal plan the ablation zone was an average of 0.5cm larger than the plan. “We did not control for respiration”, Ziemlewicz commented, “so we knew that these would be elongated in the coronal plane”. In terms of targeting tumours, the investigators report a 90.9% success rate—one of the eleven tumours treated was mistargeted immediately adjacent to the 0.5cm tumour. Ziemlewicz ascribed this mistargeting to poor ultrasound visualisation, and explained that the patient is set to undergo a second procedure for local control.
Concerning safety, there was one Grade 4 adverse event (classified as life-threatening, with urgent intervention indicated), which Ziemlewicz explained was not thought to be device-related. The patient was admitted to hospital and the complication was attributed by the independent treating physicians to their underlying Crohn’s disease. In addition, there was one Grade 2 (designated as a moderate complication) adverse event, which was also not attributed to the device. This patient was admitted to hospital for fever and given supportive treatment. One patient had a complication that was device-related; a Grade 1 (mild) adverse event, they presented with post-ablation syndrome one day after the procedure and had a fever of 39°C. This patient was the only one of the eight to have three ablative treatments; 64mL of total ablation. “They had a fever and some malaise for a couple of days after the procedure, which resolved and they are doing fine [now]”, Ziemlewicz assured the audience.
The deepest tumour treated by the study investigators did experience some local progression. Explaining this, Ziemlewicz said: “The prototype transducer we used is only capable of treating to about 10cm; we were pushing it to the edge of the envelope [with trying to treat this tumour].” Showing the audience some post-procedural images of the patient’s liver, he commented “You can see at one month the ablation zone is nicely absorbed, and then at the three-month follow-up scan you can see the progression. One of the benefits of this technology is that you can see this relatively early.”
In terms of analgesic requirements, another of the study’s secondary endpoints, there were no analgesic requests and no reported pain.
The involution data were of particular interest to the investigators as they were unsure how this would translate from previous laboratory studies. Ziemlewicz tells Interventional News: “We did note this in our original study published in Radiology last year. We survived half of those treated animals which is where we noted this involution. We honestly were not sure how this would hold up in human livers, which were either cirrhotic or patients were treated with chemotherapy previously.”
There was significant involution after two months: an average of 88.1% volume contraction and 51.1% diameter contraction. Ziemlewicz suggested that rapid involution may allow earlier identification of incomplete treatment.
All RAST procedures (VORTX RX system, Histosonics) were performed with the patient under general anaesthesia. Speaking from the floor, John Kachura (Toronto General Hospital, Toronto, Canada) asked about this decision: “No patients reported pain afterwards, and all procedures done under general anaesthetic. Has anyone tried doing it without general anaesthetic, and just with conscious sedation, or is there concern about that?”.
Ziemlewicz replied that initially, the investigators did not know how the patients were going to feel, and decided to use general anaesthetic to stay consistent with their institution’s policy of using it for all ablation patients. He did say, though, that “Anecdotally, none of the patients showed any vital sign changes to suggest they were having pain during the procedure. […] In the future, we will definitely consider doing this with conscious sedation”.