Percutaneous CT-guided radiofrequency thermal ablation is a safe and effective alternative treatment option in patients with pulmonary metastases from hepatocellular carcinoma (HCC) that cannot be considered potential candidates for surgery. This is the result of a retrospective study by Italian investigators, presented at the European Conference on Interventional Oncology Annual Meeting (ECIO; 22–25 April, Vienna, Austria) by Giulia Lassandro (University Federico II, Department of Advanced Biomedical Sciences, Naples, Italy).
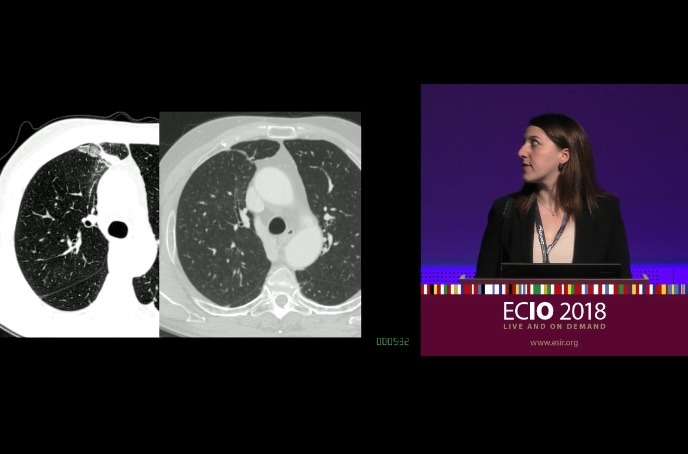
The study investigators performed a retrospective evaluation of overall survival, local tumour progression, complication rates and early outcomes of percutaneous CT-guided ablation of pulmonary metastases from HCC. HCC is the most common primary tumour in the liver, representing about 90% of primary liver malignancy, and is the third leading cause of cancer-related mortality worldwide. The most common site for HCC metastases is the lungs. In fact, Lassandro informed the ECIO audience that pulmonary metastases occur in 55% of cases via haematogenous dissemination to the pulmonary capillary network.
From February 2012 to September 2017, a total of 23 patients underwent CT-guided radiofrequency thermal ablation treatment as a first line therapy. There were 13 males and 10 females, with a mean age of 62 years. There was a total of 38 lung lesions, treated in 36 CT-guided ablation sessions (two patients had two metastases treated during the same procedure).
Of the 23 patients treated in this study, overall survival observed at one year was 87%, 67% at three years, and 44% at five years. If HCC is untreated, the average survival rate is less than six months. The investigators also report a low complication rate for radiofrequency thermal ablation. The most frequent complication observed in their patient cohort was subtle pneumothorax, which occurred in six of the 38 lung lesions (16%). Just one patient experienced a pneumothorax requiring pleural drainage tube insertion. The most dangerous complication observed was a relapse on a treated lesion, which occurred in one patient who died of extensive HCC occurrence in the liver.
Lassandro comments, “In general, patients with pulmonary metastases may benefit from surgical therapy, but current usual practice for metastasectomy is limited to a specific subset of patients, meaning that the vast majority of them are not suitable for resection. As an alternative, these patients could be treated with minimally invasive therapies like radiofrequency ablation, microwave and cryoablation, that preserve an effective lung parenchyma and have already been used in the treatment of lung lesions.
“In our experience, radiofrequency thermal ablation improves survival and quality of life in selected patients when used in addition to medical therapy.”
Fielding questions from the ECIO audience, Lassandro was asked how she was able to convince the oncologists in her hospital to allow her to perform ablation in metastatic HCC patients. Lassandro answered: “I am very lucky, because at my centre we have a tumour board, including oncologists, pneumologists, gastroenterologists, diagnostic radiologists, interventional radiologists, and also a surgeon. So generally, we treat these type of patients—selected ones with no sign of hepatic disease—with radiofrequency ablation. But it is not a rule for us, because generally oncologists want to treat them [metastatic HCC patients] with Sorafenib. But we do not stop Sorafenib during the RFA treatment, so generally we accord with our oncologists to do this type of treatment in patients with continuous medical therapy. So we agree with each other on this type of treatment on our tumour board.”
Study details
The mean size of the pulmonary metastases was 14mm, with a size range of 30–40mm. None of all 23 patients had active HCC foci in the liver, and no more than three metastases in the lung at the time of radiofrequency thermal ablation treatment. Follow up visits were scheduled at one, three, six, 12, and 24 months after treatment, and each follow-up appointment included a physical examination, protein assay, liver function tests, and also a tumour recurrence monitoring by CT scan.
According to the Barcelona clinic liver cancer (BCC) flow chart, all of the patients included in this study were metastatic, and were classified as advanced stage C. They were treated with Sorafenib in addition to radiofrequency ablation. Every patient was also classified as Class A in the Child-Turcotte-Pugh score, as they had not sign of advanced hepatic disease and no alteration in functional liver tests.
To evaluate treatment effectiveness, the study investigators used contrast CT to detect enhancement and dimensional changes in the lesions. Over the five-year study period, Lassandro and colleagues used three different devices to perform the ablation procedure.













