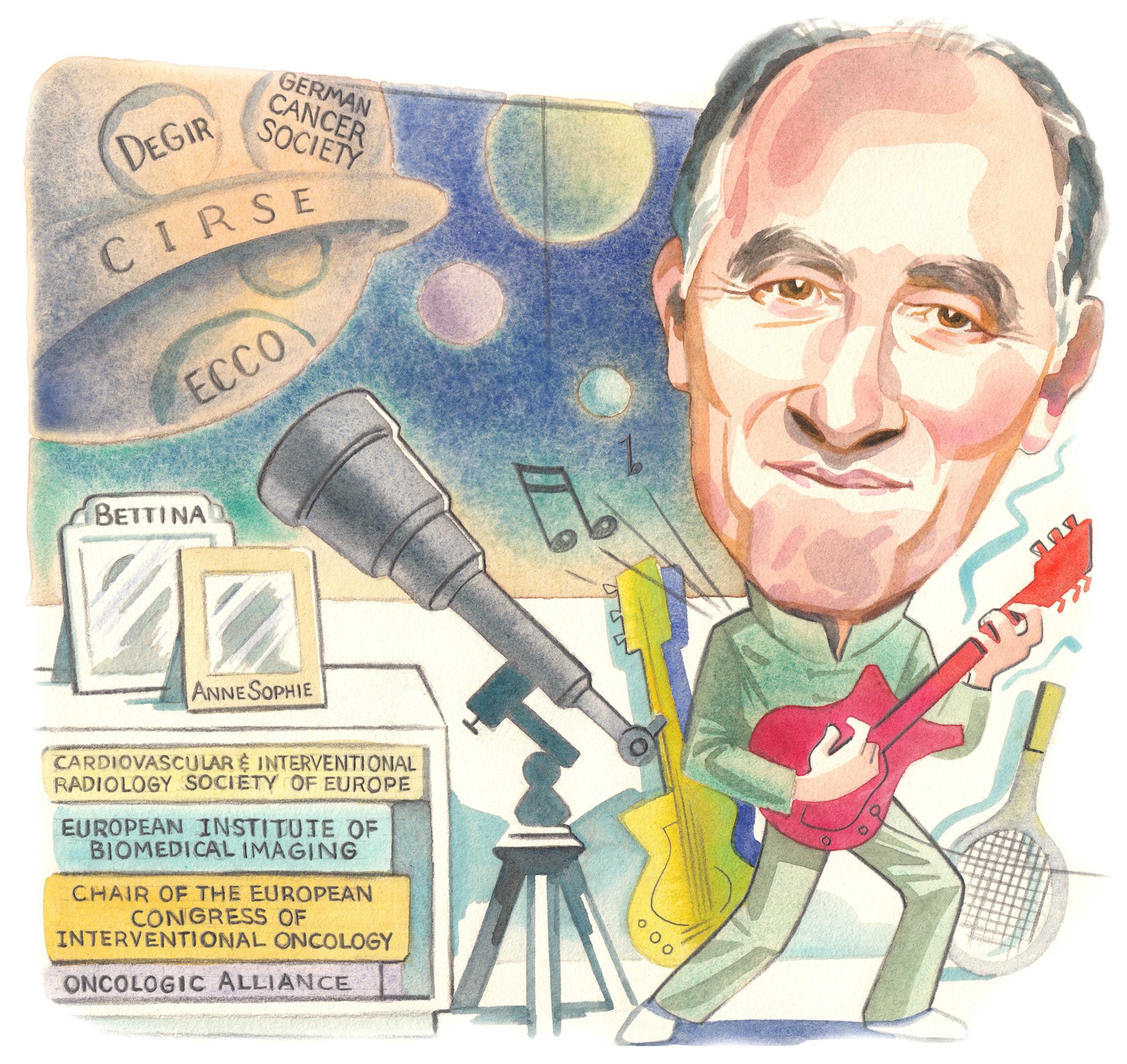
 Chair of the 2022 and 2023 European Conference on Interventional Oncology (ECIO), Philippe L Pereira muses on the status of interventional oncology (IO) in 2021, following more than a year of disruption from the ongoing COVID-19 pandemic. Through his work on various European guidelines delineating cancer care pathways, he has been instrumental in shaping the discipline and flying the flag for IO within multidisciplinary working groups. “Most oncologists recognise the value of our minimally invasive therapies and know very well how to integrate our treatments into the therapeutic armamentarium that currently exists for cancer patients,” he says.
Chair of the 2022 and 2023 European Conference on Interventional Oncology (ECIO), Philippe L Pereira muses on the status of interventional oncology (IO) in 2021, following more than a year of disruption from the ongoing COVID-19 pandemic. Through his work on various European guidelines delineating cancer care pathways, he has been instrumental in shaping the discipline and flying the flag for IO within multidisciplinary working groups. “Most oncologists recognise the value of our minimally invasive therapies and know very well how to integrate our treatments into the therapeutic armamentarium that currently exists for cancer patients,” he says.
What initially attracted you to a career in interventional radiology?
My mother wanted me to go to law school, my father preferred business, so I decided to become a doctor! No, in actual fact, as far back as I can remember, I have always wanted to be a doctor. That said, I wanted to be a psychiatrist, and I am now on the other side of medicine, the more technical side. Why interventional radiology (IR)? IR, well, because I like the operational side and being able to have an immediate influence on the disease, so as to help patients as soon as possible—the diagnosis alone without the interventional side would never have satisfied me. What we do as interventional radiologists is just incredible.
Who have been important mentors throughout your career?
Alain Roche would be the first one I would like to mention: I did not work with him for very long, but it was his enthusiasm that convinced me that IR was what I wanted to do in my life. The mentor I have learned the most from in the angiographic room was my colleague in Tübingen, Germany, Peter Huppert. One day, he brought back a radiofrequency generator that he had in his office; I quickly recognised the huge potential of this technology, and I have been using this therapeutic modality since 1996. I would also like to thank two other mentors who helped me a lot with their ideas: Fritz Schick, a physicist, and Claus Claussen.
As chair of the 2022 and 2023 ECIO meetings, what are the main takeaways you want for attendees?
First of all, I hope it will be a physical meeting, in person, and a great event to attend. It is a great honour for me that my European colleagues offer me this important position. My main purpose for this meeting is to emphasise the importance of clinical and pre-clinical studies, and to provide all possible support, starting from having the right idea—i.e. the study that will advance IO—then defining the design of the clinical study, right up to its funding. We will also highlight the multidisciplinary nature in the care of cancer patients: we are fortunate to include an oncologist, a surgeon, and a radiotherapist in the scientific programme committee (SPC). We also aim to cover the role that IO can play in combination with new immunological therapies, and to help define the contribution of artificial intelligence (AI) in our daily practice. All this will make ECIO 2022 an exceptional event.
How has the COVID-19 pandemic impacted medical conferences?
At the beginning of the pandemic, I thought that many conferences would become “digital”; I no longer think so. I feel that colleagues need to meet and discuss their latest experiences in person, candidly exploring the latest innovations or their most recent cases, discussing why they did not work as expected or how they achieved such success. Nevertheless, this pandemic has stimulated us, forcing us to find new options to continue education and research. We will probably keep some of these options and make our meetings a kind of hybrid, with sessions that may be live (in person) or half-live (also available digitally).
You are also a member of the Oncologic Alliance subcommittee. What sort of work does this do?
Yes, under the leadership of Andy Adam, this Alliance is addressing, among other things, the recognition of IO, defining international criteria for quality of cancer care, helping to design working groups to explore new and complex aspects of cancer care, and supporting the role of interventional oncology. The list of activities we undertake goes on and on.
You have also been involved with the development of European guidelines related to cancer management. What are the most important considerations when designing new guidelines?
This is a question for which I would need a full journal to answer! When you are working on new guidelines, you need to know all the results of the clinical studies in order to get the best recommendations for the patients. This is a particularly complex job, as you also need to know the results obtained by other medical disciplines as well as those from your own specialty. In cancer care, you have to recognise and support the interdisciplinary aspect: no one has a monopoly on the ideal treatment alone. These collaborations are very important, firstly to define the best treatments for our patients, and secondly to secure (and defend) the position of IR. As we do not have the resources of the pharmaceutical industry for large randomised studies, we need the results of our treatments in large, prospective and controlled registries, which also have the advantage of presenting “real-world” results with a good level of evidence.
What has the experience been like working with the European Cancer Organisation to establish a European network for interdisciplinary research on the diagnosis and treatment of oncologic diseases, and why is this international collaboration so important?
My experience is in fact very positive: IO has found its place in most guidelines, and this is in the interest of the patients. Most oncologists recognise the value of our minimally-invasive therapies and know very well how to integrate our treatments into the therapeutic armamentarium that currently exists for cancer patients.
What developments in IO are you most excited about?
IO is one of the most fascinating and promising specialties in medicine. To mention just a few aspects, I would like to emphasise the extraordinary opportunity that we must seize as interventional oncologists working in what we refer to as “the era of personalised medicine”. There are few medical disciplines that are as patient-oriented as ours. Each therapy is individualised: the application, the doses of drugs that are applied under imaging control, the change of therapies, and the possibility to combine our treatments with systemic treatments, surgery, or even radiotherapy.
Another key development is the enormous interest in new targeted therapies in the immunooncology space. Who can deliver these new therapies more locally than interventional radiologists? Another is to boost the immune response by combining our local treatments with systemic therapies. This is a great opportunity for our specialty. The interventional radiologist can be at the centre of this evolution, at least for some cancers in selected patients, if we are able to participate in preclinical and clinical studies. I say participate and unfortunately not lead because I must admit that we are not the first doctors to be contacted by the pharmaceutical industry.
To achieve this recognition we need first to make IR known to medical students (what could be more attractive than combining minimally-invasive treatments with minimised instruments, intelligent programmes, 3D images, and artificial intelligence). Second, we need to increase our influence in the education of young colleagues, to further the development of experts, and to be able to offer IO services in the same way that surgeons offer surgery: in all hospitals, not just in some specialised centres. Several scientific societies, such as the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), are working hard on this.
What is the greatest challenge currently facing interventional radiologists?
Our position is much better recognised than it was 20 years ago, but there is still a lot to do. The main challenge is to establish IO truly as one of the four pillars of cancer care. It seems to me that it is less necessary to convince oncologists—good oncologists know the benefit we can bring to patients—than it is to inform them of what we can do in the first place. Still too many oncologists are not aware of the wide spectrum of treatments we have to help cancer patients.
Another challenge I would like to mention here is the need to conduct good prospective clinical studies and to stop with retrospective studies on small cohorts that are generally not recognised for guidelines. Again, personalised medicine is a huge opportunity for interventional oncology.
What are your hobbies and interests outside of medicine?
I have a fantastic daughter, Anne-Sophie, of whom I am very proud, and with whom I try to make up for (past) lost time, and my wife, Bettina, with whom I have so many things in common. When I have some spare time, I take one of my electric guitars and play Hendrix, Led Zeppelin, Clapton… or at least I try to! My secondary hobby is definitely sports: tennis, jogging, and rowing, at least twice a week. When it rains, my reading is mostly focused on astronomy, from GNz11 to the acceleration of the universe and the quintessence!













