The late mortality risk associated with paclitaxel-coated balloons and stents when used in the femoropopliteal arteries for the treatment of peripheral arterial disease (PAD) is lower than initially reported, as investigators incorporate more patient-level data into the analysis, but the signal persists nonetheless. This is the finding of a new meta-analysis presented by independent researchers from VIVA/NAMSA at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting (25–29 September, San Francisco, USA).
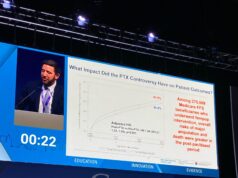
The latest data from the independent, patient-level analysis showed a mortality risk (HR 1.27, 95% CI 1.03–1.58) “incrementally” lower than the last update from the US Food and Drug Administration (FDA) device panel convened in June this year (HR 1.38, 95% CI 1.06–1.80), Krishna Rocha-Singh (Prairie Heart Institute, HSHS St John’s Hospital, Springfield, USA) told the TCT audience.
“This updated meta-analysis, which represents the most comprehensive analysis of available individual patient data to date, demonstrated a modest and consistent mortality signal in patients exposed to paclitaxel. However, it did not identify any explanation,” he said.
On 6 December 2018, Konstantinos Katsanos (Patras, Greece) and colleagues published a meta-analysis in the Journal of the American Heart Association (JAHA) reporting an increased association of mortality when paclitaxel devices were used in the leg to treat PAD patients. The mortality signal they found was HR 1.93. Amongst the ongoing international conversation spawned by the publication of these data were criticisms of the lack of patient-level data in the original JAHA meta-analysis. Industry stakeholders and the FDA started working to gather individual-level data.
Today, the paclitaxel device issue is “by no means a done deal” and has “taken over the majority of our work load,” Eleni Whatley, of the FDA, reportedly said at TCT. She informed the audience that any new application for a device containing paclitaxel has to apply at least five years of data and have minimal loss to follow-up.
In June this year, the FDA panel concluded that devices already on the market should remain available given their risk-benefit ratio, but agency advisors also called for a change in labelling. Whatley said at TCT that this was imminent, to be expected in the next few weeks.
No mechanism for increased mortality has been shown.
Rocha-Singh summed up: “The updated met-analyses [sic], which represents the
most comprehensive analysis of available IP [individual patient] data to date, demonstrated a modest and consistent mortality signal in patients exposed to paclitaxel, however, it did not identify an explanation. Consideration of ‘real world evidence’, although hindered by issues of reliability, lack of follow-up, selection bias and internal controls, may offer insights [into] paclitaxel device use and mortality.”