President-elect of the Society of Interventional Oncology (SIO), Matthew Callstrom discusses his journey into cancer care, and how advances in percutaneous ablation have shaped the procedure’s integration into first-line therapy. “If we [interventional oncologists around the world] can work together to achieve common standards, we will be able to develop evidence to support interventional oncology [IO] procedures in guidelines at an earlier point in a patient’s care,” he says.
What initially drew you to interventional radiology, and then more specifically interventional oncology?
The opportunity to improve the care of patients through interventional radiology and IO by offering minimally invasive treatments that reduce pain and morbidity and also improve survival continues to motivate me. I strongly believe that what we offer patients is often a significant improvement over surgery and other treatment options.
Who have been important mentors for you throughout your career?
I was fortunate to have mentors that were advancing the care of patients in the very earliest days of IO. Both Bill Charboneau and Luigi Solbiati were great role models for driving improved care of patients with new, innovative technology and supporting the advancement through scholarship. They were instrumental in promoting an international approach to sharing lessons learned and advancing the care of patients with cancer.
As president-elect of the SIO, what are your hopes for the society over the next year?
The primary goal over the next year will be to work with the SIO leadership and membership to help advance the clinical evidence that demonstrates the value of IO for patient care. The SIO is focused on advancing the care of patients through supporting both investigator-initiated feasibility studies but also through pivotal clinical trials, industry partnership, and advocacy for IO. We are also committed to improving the care of patients by advancing IO through guidelines and standards.
You were very involved in the World Congress of Interventional Oncology (WCIO) 2013–2017. Could you describe the transition of WCIO to SIO: Why was this necessary, and what has SIO been able to achieve that a congress alone could not?
The WCIO was a great format for communication of the advances of IO, but it was only a meeting. The transition to a society and SIO was to build the support of education, research, and advocacy that expands the impact of the physicians and industry partners committed to IO. A good example of what SIO has accomplished is the support of teams that update the National Comprehensive Cancer Network (NCCN) guidelines on a regular basis. Another benefit of a society is the support of research efforts that advance the science of IO. If you look back at the history of radiation oncology, the formation of the Radiation Therapy Oncology Group (RTOG) was instrumental in advancing the evidence that supports the use of radiation therapy for patients with cancer. SIO is working to support IO through a similar infrastructure.
As a Section Editor of Cardiovascular and Interventional Radiology, what makes a good research paper, in your opinion?
I think a good research paper is focused on advancing the care of patients with clear communication of the findings. While early experience of new applications or advances is important, we need to produce evidence that shows how IO is important for patient care. It is important to recognise that decisions at tumour boards are driven by high-quality data with an emphasis on phase II/III studies.
Could you describe a particularly memorable case of yours?
I have been fortunate to be involved in the care of patients that have had improved survival due to the care that we provide in our practice. I was part of the team treating a patient that had metastatic hepatocellular carcinoma (HCC) but survived more than 10 years due to the care we provided. He had more than 10 ablation treatments involving his liver, adrenal, lung, spine, and body wall. Throughout the time that we cared for him, he continued in his medical practice and his son became a teenager. We developed a great friendship and I attended his funeral with his passing, which was difficult, but the celebration of his life at the service was a profound experience for me.
With your particular expertise and interest in percutaneous ablation, what do you think is currently the most exciting research involving this procedure?
I think we are now at the point in the use of ablation procedures where integration in first-line therapy has an important role. We have established that local control with ablation is complementary and comparable with surgery and radiation therapy for some applications. I think that in the next few years we will demonstrate that ablation procedures offer the advantage of tissue preservation and less morbidity over the course of a patient’s life with cancer. There is also promising research that ablation in combination with immune therapy may provide abscopal response for patients with metastatic disease.
How do you think the COVID-19 pandemic has influenced IO, over the short- and long term?
We experienced a continued need for the treatment of patients with cancer throughout this pandemic. We initially reduced our access in order to implement safety measures such as measuring aerosol clearance in our procedural suites and improved standards for personal protection equipment. We learned that we can safely offer cancer treatments with appropriate testing. We learned the necessity of continuing to offer treatment for patients rather than attempting to prioritise only for more acute or semi-acute patients as delayed care is a risk to patients for progression and potentially survival.
Which innovations have most influenced your career, and how?
The introduction of improved ablation devices has allowed better outcomes for IO treatments. The first heat-based devices we used were underpowered, and getting a complete treatment was often difficult. Percutaneous cryoablation devices have allowed the expansion of treatments that we can offer. I was involved in the use of the intraoperative liquid nitrogen systems many years ago and, although innovative, treatment of renal masses, lung tumours, and musculoskeletal tumours would not be possible. We now treat more than 500 patients a year with this technology. Hybrid rooms are also putting the best imaging methods in the hands of the proceduralists, allowing both CT and fluoroscopy imaging, where they offer the best visualisation and guidance approach.
What are the biggest challenges facing IR today?
I believe we need to work together to improve the standard performance and delivery of IO treatments. Many of the procedures that have matured and are helpful for patients are done differently in centres across the world. We have been involved in multicentre clinical trials where we have struggled to gain a common approach in the use of devices and technical performance, and the outcomes have been impacted negatively. Performing procedures with standard approaches and objective outcomes will both advance patient care and elevate the standing of IR/IO in the world. If we can work together to achieve common standards, we will be able to develop evidence to support IO procedures in guidelines at an earlier point in a patient’s care.
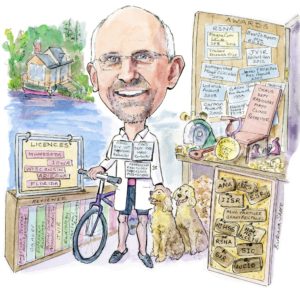
What are your hobbies and interests outside of medicine?
Outside of medicine, I am blessed to have a wonderful family, including my wife Brenda and my two boys, Joseph (30) and Peter (27). We also have two golden doodles (Charlie and Lucy) that are our constant companions and treated like children now that we are empty nesters. We spend as much time as we can at our lake cabin that is on the lake that Brenda and I first met and honeymooned—our family and friends often join us, and although there are 10,000 lakes in Minnesota, there is only one as far as our family is concerned. I enjoy making furniture in my wood shop even though there is usually more dust than any final product generated. I also enjoy riding a road bike—on the less travelled roads near our house and cabin, and in the basement on a trainer during the too-long winters in Minnesota.













