This article is sponsored by BD.
In a complex patient population with advanced, symptomatic below-the-knee peripheral artery disease, treatment with the Lutonix drug-coated balloon (BD) led to excellent freedom from all primary safety endpoints, including 30-day all-cause death, above-ankle amputation, and major reintervention. These interim real world data of the Lutonix global drug-coated balloon registry at 12 months, were presented by Dierk Scheinert (Leipzig, Germany) at the Cardiovascular and Interventional Radiological Society annual meeting (CIRSE; 22–25 September, Lisbon, Portugal).
In the prospective, multicentre, single arm Lutonix global registry, 371 infrapopliteal lesions were treated with the Lutonix drug-coated balloon (DCB). Patients were Rutherford category 3, 4 or 5; two-thirds were diabetics, three quarters suffered from critical limb ischaemia (CLI), and 65% were Rutherford category 5. Mean lesion length was 12cm, with over 20% exhibiting severe calcification.
The interim data presented by Scheinert at CIRSE is highly promising. Out of 244 patients, only 5.4% had a major amputation within one year, a result which Scheinert describes as “very reassuring for this complex patient population.” All-cause mortality was around 12% after one year of follow-up, and there were no unexpected device related events reported. Furthermore, there was 99.7% freedom from re-intervention for distal embolization in the patient cohort.
Improvement in Rutherford clinical category (RCC) was also marked: 80% of patients exhibited a clinical improvement by≥1 RCC, and almost two-thirds demonstrated an improvement by≥3 RCC.
“As the clinical outcome is of utmost importance for the patient,” Scheinert says, “I was most surprised by the excellent clinical results with improvement of Rutherford clinical category in 80% of patients. Further, the observed 80% freedom from target lesion revascularisation rate at one year is very promising, as patency failures are observed frequently after infrapopliteal interventions, in particular in diabetics and CLI patients.”
Speaking to Interventional News of the results’ significance, he states, “Patients with below-the-knee (BTK) disease suffer from high failure rates with currently available treatment modalities, as standard balloon angioplasty for long, complex infrapopliteal lesions is limited by high restenosis rates. As innovations are urgently needed, the Lutonix DCB could become a new tool to improve outcomes in this special patient population. Of course, the results of the Lutonix below-the-knee randomised trial are highly anticipated, and final results of both studies could have a major impact on clinical practice.”
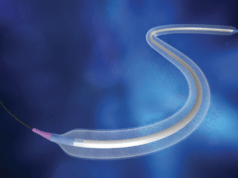
The Lutonix DCB is coated with excipients polysorbate and the endogenous metabolite sorbitol, as well as paclitaxel at a density of 2μg/mm2. Extensive in vitro and in vivo testing has previously demonstrated an excellent downstream particulate safety, with minimal risk of embolization. Scheinert explains how this is particularly important in BTK interventions, where compromised outflow to the foot arteries is often present. He further explains how “a good balance was achieved between adhesion of the coating to the balloon during handling and advancement to the lesion and release of the coating to the vessel wall upon deployment”.
According to Scheinert, patients with long infrapopliteal lesions may benefit most from treatment with the Lutonix DCB, “as restenosis rates are high, especially in diabetics.” Importantly, he notes that target lesion revascularisation rates were comparable for diabetics and non-diabetics.
Recruitment for BTK studies is typically difficult, as patients are often older, suffering from multiple co-morbidities. Ensuring follow-up is also a major challenge, lending greater significance to the results of the present study.
Scheinert also emphasised the importance of using real world registries, arguing “results from real-world patients are important to ensure safety and efficacy of new devices for all treated patients”.
So far, an extensive clinical trial programme showed the benefit of using a Lutonix DCB in the treatment of obstructive lesions in the superficial femoral artery, while confirming minimal risks with the addition of the drug compared to standard balloon angioplasty. Now the same formulation is under investigation for BTK patients and the vascular community eagerly awaits the results of the Lutonix randomised trial, anticipating a potentially major impact on current standard care. Based on his presentation Scheinert summarises: “As these first results are promising, we hopefully can add the Lutonix DCB to our armamentarium for below-the-knee interventions soon.”