Histotripsy is a non-thermal, non-ionising and non-invasive focused ultrasound technique which relies on cavitation for mechanical tissue breakdown at the focal point. Leading research into the novel technique, Mishal Mendiratta-Lala (University of Michigan, West Bloomfield, USA)—principal investigator for the #HOPE4LIVER trial evaluating histotripsy in liver tumours— provides a deep dive into histotripsy, discussing its application and evolution in the near future.
In 2024, histotripsy has advanced significantly following its US Food and Drug Administration (FDA) approval in late 2023, allowing many institutions to acquire the technology for clinical use. Most systems were delivered this year, leading to the treatment of over 500 tumours with histotripsy.
Although enthusiasm is high among both patients and the medical community, it is still too early to report definitive new findings. The focus must remain on collecting and analysing data to assess long-term efficacy. A key priority moving forward is careful patient selection, ensuring that histotripsy is used appropriately rather than broadly applying it to all cases.
Histotripsy garners “excitement” in the cancer community
For patients deemed suitable for treatment with histotripsy, the procedure has demonstrated several benefits over alternative ablative techniques. These are largely due to the non-invasive nature of the procedure, minimal bleeding risk, and post-procedure pain and recovery times.
There is excitement in the cancer community about histotripsy’s potential to induce an abscopal response— a systemic immune reaction against cancer. However, this effect has not been reliably observed in clinical practice yet and we look forward to emerging research that may bear out evidence of this response.
Current data supporting histotripsy’s efficacy is limited but promising. To date, there are two peer-reviewed studies that are analysing histotripsy—the first-in-man THERESA trial evaluating histotripsy of hepatic tumours, and the #HOPE4LIVER trial which concerns the treatment of liver tumours with histotripsy. The former is a small early study focused solely on safety. The 36-hour data confirmed that treated volumes were effectively ablated, demonstrating initial safety. The latter #HOPE4LIVER trial involved 44 tumours and evaluated 30-day safety and efficacy. The results showed that histotripsy successfully treated the target lesions, with no enhancement of the treated tumours, confirming short-term efficacy.
These studies confirm that histotripsy is safe, but long-term efficacy, survival benefits, and recurrence rates remain unknown. To determine whether histotripsy improves overall survival and delays disease recurrence, more clinical trials and data-sharing across institutions are essential. Treating patients with only 30-day data in 44 tumours is premature for broad clinical adoption, emphasising the need for further research.
“Challenging” operator learning curve
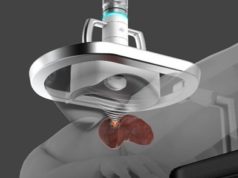
Leading histotripsy technology innovation, the Edison (HistoSonics) platform has a notable operator learning curve due to its complexity and multiple components requiring proficiency. Challenges include setting up the water bath correctly to prevent leaks, accurately identifying the target, and properly defining treatment boundaries. The robotic head’s large and bulky design adds difficulty in positioning for optimal lesion treatment. Additionally, treatment limitations arise from factors such as lesion depth, adjacent structures, and device voltage constraints.
As for institutional implementation, while the platform can be highly effective when the target is appropriately selected, its adoption requires significant training, experience, and institutional investment in both personnel and infrastructure. Proper training programmes and support are essential for successful integration. I believe a successful histotripsy programme requires institutional commitment and resources, making it challenging to adopt easily.
While institutions can integrate the technology, its success will depend on the presence of a strong clinical team, institutional support, a general anaesthesia team, adequate space and finally, a financial bolster. Insurance reimbursement is not always guaranteed, and thus institutions will need a strong financial team to navigate funding and advocate for coverage.
What’s to come for histotripsy in 2025
The year 2025 will be an exciting one for histotripsy as the field evolves. With more institutions purchasing the device, the accumulation of clinical data will be crucial. However, the success of histotripsy will depend on strong collaboration within the clinical community to analyse outcomes and refine patient selection criteria. Not all patients will be ideal candidates, making ongoing clinical trials essential for optimising the technology’s impact in cancer treatment.
Global adoption of histotripsy is likely to grow, but its integration into standard care will require further validation through research. We need more clinical trials with combination therapies and we need more trials looking at treatment of different cancer types.
A key focus for 2025 will be ensuring that histotripsy is implemented effectively and safely. Additionally, while the potential for an abscopal response is intriguing, it remains unproven in patients, and caution is necessary to avoid unintended consequences.
In addition, histotripsy is being expanded to renal and pancreas applications which will be very exciting. Overall, histotripsy has significant promise, and 2025 will be a pivotal year in determining its role in the broader clinical landscape. The medical community plays a critical role in shaping the clinical narrative and ensuring responsible treatment decisions. Looking ahead, I hope to be able to lead clinical trials, which will be essential in identifying the ideal patient population and determining whether histotripsy can provide meaningful survival benefits for cancer patients.
Mishal Mendiratta-Lala is an interventional radiologist at the University of Michigan in West Bloomfield, USA.