 Results from a multicentre, randomised controlled trial—FEMME—published today in the New England Journal of Medicine (NEJM) indicate that myomectomy shows superior fibroid-related quality of life at two years compared to uterine artery embolization (UAE) in women with symptomatic uterine fibroids. Several prominent interventional radiologists suggest that while gynaecologists may use this headline finding to cease recommending UAE, the treatment is still a good therapeutic option in patients with symptomatic fibroids. They highlight that informed patient choice is at the heart of personalised fibroid therapy.
Results from a multicentre, randomised controlled trial—FEMME—published today in the New England Journal of Medicine (NEJM) indicate that myomectomy shows superior fibroid-related quality of life at two years compared to uterine artery embolization (UAE) in women with symptomatic uterine fibroids. Several prominent interventional radiologists suggest that while gynaecologists may use this headline finding to cease recommending UAE, the treatment is still a good therapeutic option in patients with symptomatic fibroids. They highlight that informed patient choice is at the heart of personalised fibroid therapy.
Isaac Manyonda (St George’s, University of London, London, UK) and colleagues’ publication coincides with fibroid awareness month. July 2020 has seen healthcare workers, hospitals, and other organisations promoting uterine health, shining a spotlight on an underexposed condition that one in three women will experience in their lifetime.
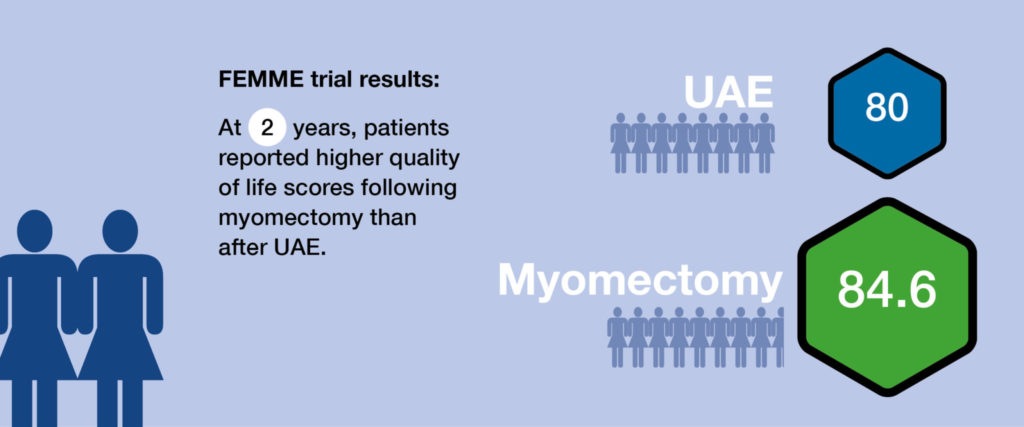
The triallists set out to compare the effect of UAE and myomectomy on quality of life in women with symptomatic fibroids wishing to avoid hysterectomy. The primary outcome measure of the FEMME trial (Fibroids with embolization or myomectomy to measure the effect on quality of life) was the condition-specific quality of life domain score from the Uterine Fibroid Symptom Quality of Life questionnaire (UFS-QOL). Scores could range from 0–100, with higher numbers indicating a better quality of life.
Average quality of life scores at two years were substantially improved in both groups, but were greater in those assigned to myomectomy (mean-adjusted difference using complete case analysis: eight points; 95% confidence interval [CI], 1.8–14.1; p=0.01; mean-adjusted difference with missing responses imputed: 6.5 points; 95% CI, 1.1–11.9). Mean quality of life score at two years from randomisation was 84.6±21.5 in the myomectomy cohort, versus 80±22 in the UAE group.
In total, 254 patients were recruited from 29 hospitals, and randomly assigned to undergo myomectomy or UAE as the primary procedure in a 1:1 ratio. Women were only eligible for enrolment if they were considered suitable for either procedure.
“The six- to eight-point benefit on average in health-related quality of life scores in the myomectomy group, as compared with the UAE group, is consistent with small to moderate standardised treatment benefit at two years,” the authors write. “However, the 95% confidence interval around these estimates indicates that plausible results range from almost no benefit of myomectomy over embolization to a moderate (15 point) difference.”
Despite the increased quality of life scores in the myomectomy cohort, several interventional radiologists, including two of the study co-authors, have expressed to Interventional News that UAE is still a good option for patients with symptomatic fibroids. Jonathan Moss (University of Glasgow, Glasgow, UK), a co-author of the NEJM study, comments: “Although the quality of life was higher in the myomectomy group and [this difference was] statistically significant, it was only a few points better. Therefore, provided women understand this, then they can choose either procedure.”
Fellow study author Anna-Maria Belli (St George’s University Hospital NHS Foundation Trust, London, UK) echoes this sentiment, telling this newspaper that “The results show a substantial benefit to treatment in both groups with regard to quality of life and symptom severity, even though the results for myomectomy were better than UAE.” However, she adds that she believes “The results do not mean UAE is an inferior treatment to myomectomy.
“With regard to menstrual blood loss, the results in both groups were comparable. This means that women should be offered either treatment and choose for themselves. For some women, avoiding a general anaesthetic, having a shorter hospital stay, and avoiding an open surgical procedure (the majority of myomectomies in FEMME were open abdominal as fibroid and uterine sizes were large) is of paramount importance, in which case UAE would be their preferred option.”
Gerard Goh (The Alfred Hospital, Melbourne, Australia) also enumerates the benefits of UAE: “Individualised medicine, i.e. tailoring treatment to the patient, is an important part of patient care and as interventional radiologists we are able to offer patients an alternative treatment to surgery. Even before the FEMME trial was published, we knew that there were some patients better-suited to myomectomy, and some better-suited to UAE. Some benefits of UAE are its ability to be performed under conscious sedation, as well as a shorter recovery time that may be better-suited to young women with busy family and work commitments.”
Contextualising the investigators’ decision to use UFS-QOL score as the primary outcome measure, Moss explains that quality of life measurements are “included in almost all randomised controlled trials [RCTs]”. Early UAE trials, such as REST and EMMY (from Scotland and The Netherlands, respectively) used the SF36 questionnaire, which Moss describes as a “generic quality of life instrument”.
Weighing in on the primary outcome measure of the FEMME trial, James Spies (MedStar Georgetown University Hospital, Washington, DC, USA) comments: “The primary outcome was the change in quality of life, and the quality of life scores of the myomectomy patients were worse at baseline than the UAE group, despite the randomisation. If one looks at final quality of life scores, they are very comparable within the sensitivity of the questionnaire used, but the study was designed to use the change in scores as the primary outcome [Spies’ emphasis]. Thus, somewhat artefactually, there was a greater improvement in quality of life scores for myomectomy. If one compares final quality of life scores or symptom scores, there would have been no difference.”
The authors acknowledge that the presence of some baseline differences in health-related quality of life and age between the two groups is a limitation of their analysis, but note that prespecified analyses were adjusted for the baseline health-related quality of life, and a post-hoc analysis adjusted for age showed similar findings.
Spies describes FEMME as “an important study, one of the very few randomised trials comparing myomectomy versus UAE. It shows very comparable outcomes of both procedures in terms of symptom control, quality of life, complications, and in the limited fertility outcomes. Overall, I congratulate the authors on completing an outstanding study, which validates UAE as an effective therapy that yields comparable outcomes in this population of patients.”
UAE and myomectomy result in comparable pregnancy rates, but numbers too small to call
In terms of fertility, there were no consistent differences between groups in the FEMME trial with regard to biomarkers of ovarian reserve. Nine women in the UAE group (8%) and five women in the myomectomy group (4%) reported pregnancies within two years of randomisation, resulting in six and four live births, respectively, the authors report. However, they note there are too few pregnancies amongst the trial cohort to inform the effects of the procedures on fertility.
Expounding on the clinical implications of the two-year results, Moss relates: “We found no evidence of ovarian damage using several markers after either procedure. The number of pregnancies was low in both groups. The pregnancy data is difficult to interpret, and the intention to treat (ITT) and per protocol analysis showed no difference [between the UAE and myomectomy groups]. Interestingly, if you look at the women who actually received UAE, there were slightly more pregnancies than in those who actually had myomectomy. However, the numbers are small, and one cannot draw any firm conclusions.”
Belli believes that an “important aspect” of the trial is that the results reveal “no adverse effect on ovarian reserve from UAE, which opens up the potential for further research in younger women wishing to become pregnant”. She notes that the average age was 40 in the trial, “so low pregnancy rates are not so surprising”.
Belli adds: “Also, this trial reflects the real population of women suffering from symptomatic fibroids, with a high proportion of black women and large fibroid uteruses (mean >1,000cc).”
“There is a surprising amount of resistance from the gynaecological community across the world about offering UAE to women who wish to maintain their fertility,” Moss opines. Prior to the FEMME trial, Moss outlines how “several smaller RCTs compared these two techniques, but the numbers were small and results conflicting. Some, such as FUME, had to exclude women wishing to become pregnant. FEMME overcomes most of these problems, even though the number of pregnancies is small, with limited data on that outcome.”
He further informs Interventional News that his research team are currently considering a large trial using pregnancy outcomes as the primary outcome measure, which they believe is needed. “It would have to be a trial of several thousand women, and probably an international effort,” he says.
Other secondary outcome measures similar in both groups
In addition to fertility, other secondary outcomes measures were similar for both myomectomy and UAE: menstrual bleeding scores, peri and postoperative complication rates, and the percentage of patients who would recommend their procedure to a friend.
Specifically, at two years, the percentage of women who would recommend myomectomy to a friend was 93%, versus 84% with UAE, while respective percentages of women who said they would have the procedure again were 78% and 74%.
Peri and postoperative complication rates for both procedures were low, Manyonda et al relate, with one conversion of a myomectomy to a hysterectomy, and one conversion from a laparoscopic to an open myomectomy. At six months post-procedure, 32 of 80 (40%) fibroids treated by embolization were completely infarcted. Peri and postoperative complications from all initial procedures occurred in 34 out of 118 patients (29%) in the myomectomy arm, and in 27 out of 113 patients (24%) in the UAE group (relative risk, 1.2; 95% CI, 0.8–1.9; p=0.4).
Furthermore, a “substantially” greater number of patients in the UAE group underwent additional procedures within two years of follow-up: 18 of the 110 patients with two-year data (16%), versus eight of the 111 women (7%) in the myomectomy cohort. “This observation may be explained in part by the lower quality of life reported in the UAE group,” Manyonda et al muse. “However, more hysterectomies were performed as the initial procedure in the myomectomy group, owing either to patient preference or clinical decision.”
Moss acknowledges that the higher re-intervention rate with UAE was “a little surprising, as both procedures preserve the uterus”.
However, UAE was associated with a shorter length of hospital stay: the median time spent in the hospital for an embolization patient was two days, compared with four days for a myomectomy patient.
Belli articulates her opinion of these findings: “We knew that UAE had a greater repeat treatment rate, but the complication rate is no different between the two treatments, even though the blood transfusion and haemorrhage rate was higher in the myomectomy group. I have always believed that getting rid of the large bulky fibroids [as with myomectomy] is ultimately more satisfying for women than simply returning menstrual function and other fibroid symptoms to normal. My happiest patients were the ones who had the largest reduction in bulk, despite counselling them that this was not the main aim of UAE.”
However, reflecting on the impact of these FEMME trial data, Belli adds: “I hope that the results of this trial will make gynaecologists more accepting of UAE as an alternative, and allow a larger trial to address pregnancy rates and outcomes to go ahead. Unfortunately, I am afraid some gynaecologists might simply read the headline result and use this to confirm their prejudices and not even offer UAE.”
Moss concurs, commenting that “trying to ‘open many closed minds’ was the largest barrier” to running this trial. “At times it felt like trying to persuade someone to change their religion,” he says, “so firmly held are some views. Triallists, however, must never give up, and having a strong team, like we did, is essential.
“My message on the results it that UAE has some advantages, such as avoiding an incision, a general anaesthetic, and more rapid recovery. In my view, it is for fully-informed patients to make their own choice.”
These results will be presented at the 2020 annual scientific meeting of the Cardiovascular and Interventional Radiological Society of Europe (12–15 September), which will take place online this year for the first time.