
Complications are an inevitable component of an interventional radiologist’s practice, says Eric Keller, especially as a newer specialty with a reputation for pushing medical frontiers. As such, he elaborates on the ethics of procedural complications, and describes how he believes physicians should conceptualise and learn from their mistakes. Keller calls for more research on the ethics of complications in interventional radiology (IR), detailing how the innovation that characterises the specialty could be directed towards reimagining approaches to answering hard-hitting questions.
Some people consider “errors” and “complications” distinct, in that an error implies a mistake was made, while complications occur even when everything is done correctly. This distinction is helpful from a systems perspective, but these events do not feel very different personally or ethically.1 When a procedure does not go as expected and hurts someone, it violates a basic assumption held by patients and clinicians: doctors heal people. It leaves us with questions and uncertainty that can undermine our relationships with patients and colleagues and leave clinicians asking, “What if I had…?”. Complications seem particularly personal for interventionalists. When a patient dies on a medical service, people tend to ask, “What happened?”, but when a patient dies on a surgical service, people ask “What did you do?”.2 Although successes define one’s career, it is often responses to shortcomings that defines one’s character. Complications challenge us to be better and to support those hurt in our efforts to improve. When they occur, we should question what we owe our patients, selves, and colleagues, and to some degree, the answers are similar: reflection, confession, and resolution.
First, we should try to understand why a complication occurred and how to best avoid it in the future. It can be tempting to consider a complication merely as something that happens or attribute the fault to someone or something else, but we should always reflect upon our role in the event. Likewise, it can also be tempting to feel like a failure and let complications paralyse us, but the only interventionists that do not have complications are those that do not perform procedures. Neither extreme is helpful.
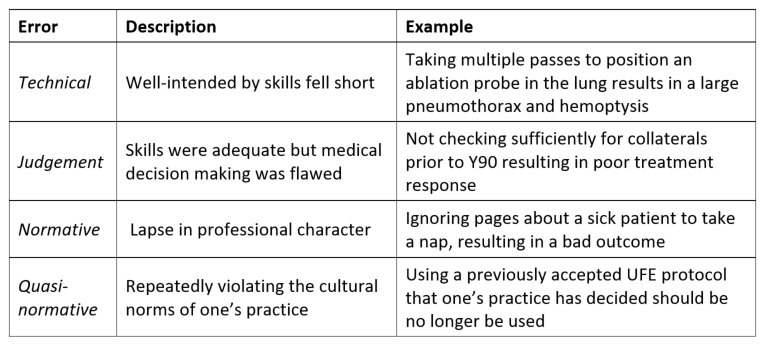
One useful approach for reflection is Charles Bosk’s categorisation of operator errors,2 which is summarised in Table 1 (below) with examples for interventional radiology (IR). Errors of technique or clinical judgement happen to everyone and are easier to improve with more training and experience. However, errors of character (normative or quasi-normative errors) are more difficult. In the face of these errors, we should look for deeper causes. Was the interventionalist depressed, burnt out, or overwhelmed by other aspects of life? Is the current practice or career not the right fit? If this is the case, we owe it to our patients, selves, and colleagues to step away and get help.
Once one has reflected upon the cause of the complication, this understanding should be used to provide an explanation and support to patients, families, and colleagues. For patients and families, complications can undermine trust, which is central to the patient-clinician relationship.3 It is trust that allows people to let us render them unconscious and thread catheters and wires into their bodies. Without this trust, it can be difficult for people to get the care they need, so in the face of complications, we owe it to patients to help rebuild that trust, not just in one clinician, but healthcare in general. Rather than abandoning patients, we should advocate for them by providing information, support, and guidance.4 An apology can also go a long way. Some may worry that an apology will increase the risk of a law suit, but research tends to suggest otherwise. Patients that sue tend to be those who did not receive the information or support they felt they deserved.5
Similarly, we should not leave our colleagues to deal with our complications alone. Rather, we should take responsibility for what occurred and partner with them. In IR, referrals networks are important, and complications can weaken these relationships. Just as with patients, we owe our colleagues an explanation and support to rebuild their trust. Colleagues can also be invaluable for stopping a difficult situation from getting worse, and we should have the humility and insight to ask for help when things go awry.6 We can also provide an opportunity for our colleagues to learn from our complications via morbidity and mortality conferences. Ideally these should be constructive and supportive rather than whipping posts for subordinates. Again, everyone has complications, and we owe it to our patients, selves, and colleagues to learn from them together.
This approach of reflection, confession, and resolution is not specific to IR, so it is also worth considering some unique aspects of IR culture related to complications. As a newer specialty, there tends to be less data to guide clinical decision making. The specialty has a reputation of being the cowboys and cowgirls of medicine, always willing to try something. We even have an entire forum to celebrate “extreme” cases that could easily end up in morbidity and mortality conferences of other specialties. This creates a complex relationship with complications. IR has classification systems to measure and report complications but not a robust forum for discussing the cases that did not save the day and how this relates to our drive for innovation or willingness to push the envelope. Furthermore, discussions of complications tend to be limited to more tangible periprocedural events such as bleeding or infection. There is little work in IR exploring issues of consent, futility, conflicts of interest, or tribalism. Overall, there seems to be a need for a balance; forums to celebrate innovation and to discuss the difficult ethical questions that interventionalists face each day.
In summary, complications and errors are likely to feel similar to interventional radiologists, their patients, and their colleagues. These events contradict expectations and hopes and leave people with uncertainty that can undermine relationships with patients, families, and colleagues. In response, we should reflect upon our complications, try to understand what caused them, and give ourselves permission to be human and learn from them. We can then use this understanding to provide an explanation and support to our patients and colleagues to rebuild trust and rapport with them. On a larger scale, we should also consider developing more research on and forums to discuss ethics in IR. Perhaps IR can develop innovative approaches to the difficult ethical questions we all face as well as the clinical ones.
Eric Keller is an interventional radiology resident at Stanford Medical School, Stanford, USA, and has a Master of Arts in Medical Humanities and Bioethics from Northwestern University, Chicago, USA.
References:
- Angelos P. Complications, errors, and surgical ethics. World J Surg. 2009;33(4):609-11.
- Bosk CL. Forgive and remember : managing medical failure. 2nd ed. Chicago: University of Chicago Press; 2003. xxv, 276 p. p.
- Pellegrino ED. Professionalism, profession and the virtues of the good physician. Mt Sinai J Med. 2002;69(6):378-84.
- Meruelo NC. Mediation and medical malpractice: the need to understand why patients sue and a proposal for a specific model of mediation. J Leg Med. 2008;29(3):285-306.
- Hickson GB, Clayton EW, Githens PB, Sloan FA. Factors that prompted families to file medical malpractice claims following perinatal injuries. JAMA. 1992;267(10):1359-63.
- Keller EJ, Crowley-Matoka M, Collins JD, Chrisman HB, Milad MP, Vogelzang RL. Fostering better policy adoption and inter-disciplinary communication in healthcare: A qualitative analysis of practicing physicians’ common interests. PLoS One. 2017;12(2):e0172865.












I really like the information which is shared in this blog about the interventional radiologist Eric Keller
Complications are an inevitable component of an interventional radiologist’s practice, says Eric Keller, especially as a newer specialty with a reputation for pushing medical frontiers and We can then use this understanding to provide an explanation and support to our patients and colleagues to rebuild trust and rapport with them. On a larger scale, we should also consider developing more research on and forums to discuss ethics in IR. Perhaps IR can develop innovative approaches to the difficult ethical questions we all face as well as the clinical ones.