French interventional radiologists are protesting the high number of “unnecessary” surgeries taking place nationwide, stressing that there are minimally invasive alternatives with fewer complications available. The Federation de Radiologie Interventionnelle (FRI), has launched a public awareness campaign to educate potential patients about interventional radiology (IR) procedures, with a specific emphasis on uterine artery embolization (UAE), which it claims is an underutilised, safe, and effective option for patients who do not want a hysterectomy. To read about this issue on an international stage, read the full coverage here.
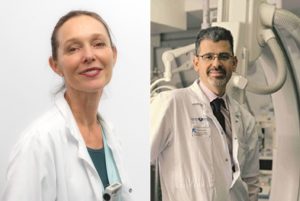
“I think gynaecologists have a real scepticism of the effectiveness of UAE,” FRI president Hélène Vernhet-Kovacsik (Arnaud de Villeneuve Hospital and Montpellier University, Montpellier, France) tells Interventional News. “They do not trust this technique, which they do not practice.”
The French guidelines for the therapeutic management of uterine fibroid tumours, published in the European Journal of Obstetrics and Gynecology and Reproductive Biology and last updated in 2012, state that “Because UAE is an effective treatment with low long-term morbidity, it is an option for symptomatic fibroids in women who do not want to become pregnant, and a validated alternative to myomectomy and hysterectomy that must be offered to patients.” However, Vernhet-Kovacsik says that though UAE is in the guidelines, and “should be offered as an alternative to hysterectomy for all patients”, it is not. On average 2,000 UAEs are performed a year in France. In contrast, 40,000 patients have hysterectomies annually.
Raising awareness
When first elected president of the FRI, Vernhet-Kovacsik set up specific working groups within the society. The communications working group, headed by Vincent Vidal (Hôpital de la Timone, Marseille, France), have launched a public awareness campaign in an effort to educate the public about UAE and other minimally-invasive options. With a focus on pelvic interventional radiology (IR) in 2020, the society’s edifying efforts are dedicated to UAE, haemorrhoids, and prostate artery embolization (PAE). As a world-leading advocate of the “emborrhoid” technique—the embolization of the superior rectal arteries—and the lead author of the 2015 study demonstrating the procedure’s efficacy, Vidal is a global specialist on haemorrhoids. PAE is the principle purview of Marc Sapoval (Georges Pompidou European Hospital, Paris, France, and founder of the GEST Symposium), who is a prominent member of FRI. UAE was chosen for more political reasons: in Vernhet-Kovacsik’s words, the lack of referrals and general awareness “seemed to us very stigmatising and unfair. How is it that a technique recognised as effective and less morbid than hysterectomy, cited in the gynaecology guidelines [and] with long established scientific evidence, remains as little used?”
The communications working group organised a press conference with French media on 23 January at the Georges Pompidou European Hospital in Paris. This resulted in a double page spread appearing in the non-specialist daily newspaper Le Parisien, featuring patient testimonials in favour of UAE, and interviews with Vernhet-Kovacsik, Sapoval, and other French interventional radiologists with private practices explaining technical details of the procedure, as well as describing how and why it is underutilised. The article cited a lack of information provided to the patient from interventional radiologists’ medical colleagues leading to a low referral rate.
Following this, Vernhet-Kovacsik recounts how Sapoval appeared on French radio to discuss embolization. “[He] brilliantly exposed the clinical and economic effectiveness of all the IR treatments, and presented emerging techniques,” she enthuses. Following the success of these media engagements, FRI produced a press kit summarising current scientific data on pelvic IR, which can be used to inform future media opportunities, in France or abroad.
“We also wanted to communicate [the impact on] quality of life,” Vernhet-Kovacsik says of the FRI media strategy, “because it has become a major concern for patients, and is an advantage of IR procedures, which have very low morbidity and require very short hospitalisations in comparison with alternative surgical techniques. This also made it possible for us to directly address patients by proposing solutions to symptoms that are not always recognised as pathological, but [are] handicapping in everyday life, such as pelvic pain or urinary discomfort.”
FRI has taken a multimodal approach to disseminating their message. The society made a short animated film about pelvic IR, which is freely available on their YouTube channel. This also hosts video coverage of radiology congresses and the preprocedural film shown to patients in waiting rooms. Additionally, Sapoval is working on a patient-facing website, to launch 13 June this year. “We are testing and finalising it now,” Sapoval tells Interventional News, “then we will be launching it nationwide. The website will inform patients of treatments for fibroids other than hysterectomy, so they can be aware that they may not need one.” FRI also plans to use Facebook to engage the online community through question and answer sessions, mediated by specialised health publications, designed to offer patients a chance to speak directly with an interventional radiologist.
This direct engagement is part of a trend Vernhet-Kovacsik has identified. “The patient-doctor relationship is changing—it is no longer directive, but participative. The dissemination of information on the web via social media and the creation of user groups should be [a step] in the right direction.” Following the increased interest in UAE that succeeded the Le Parisien article, FRI set up an online directory of pelvic IR centres in France, allowing patients to find these services more easily.
Sapoval believes this increasingly participative relationship is important because patients will have to lead the charge in advocating for UAE. “We have a very unethical situation in France where women get hysterectomies instead of embolizations because the obstetricians/ gynaecologists are operating on patients instead of referring them to interventional radiologists. This is one of the interventions where we have strong, level one evidence, and despite a lot of effort, we have not seen a lot of movement in the last few years. This is the case in many other countries as well, so we wanted to take the lead and raise the flag for UAE.”
“Some resistence” to uterine artery embolization from referrers
When questioned about why he thinks the discrepancy between hysterectomy and UAE numbers exists, Sapoval is categorical: “There is some resistance. Some [obstetricians/ gynaecologists] do not know about UAE, and some do know, but do not want to refer patients because they are paid to perform hysterectomies.”
Vernhet-Kovacsik proposes another reason for the low referral rate: “In my opinion, this goes beyond simple corporatist considerations. Women have a doctor who has looked after them for years, has helped them give birth to their children, knows their intimate problems. A recognition has been created and it is difficult for patients to dare to express desire for a treatment different to the one proposed by the gynaecologist! However, it is shocking to offer a firstline technique (hysterectomy) which has twice as many serious complications as embolization, sometimes requires transfusions, and always prolongs work stoppage. Gynaecologists’ main argument is the increased risk of embolization versus myomectomy regarding fertility, but the vast majority of patients are over 43 years old, are not keen on pregnancy, and are treated by hysterectomy and not myomectomy: so why not perform an embolization? I think our target must be this population precisely!”
UAE preserves sexual function and bodily integrity
The EFUZEN study, conducted in 2017 by Vernhet-Kovacsik, Sapoval, and others from the French Society of Interventional and Cardiovascular Imaging (SFICV) research group, evaluated sexual function before and one year after UAE. The authors concluded that at one-year post-embolization, UAE significantly improves all aspects of sexual function and quality of life. Vernhet-Kovacsik stresses the pertinence of this finding: patient’s quality of life and sexual function “are rarely addressed by gynaecologists”, she says, adding that “there is a close link between fibroids and their treatment, and these aspects of life.
“The uterus is not only used for reproduction; preserving bodily integrity is also a current demand,” she comments. “I think we should all take advantage of the ‘me too’ phenomenon and, as interventional radiologists, speak out and encourage women to dare to ask for fair treatment when it comes to preserving their femininity and their quality of life. We could certainly work together: interventional radiologists, gynaecologists, and patients. I am less concerned about the future of PAE, however technically more difficult, because the importance of preserving sexual function in men will never be questioned!”













