This advertorial is sponsored by Sirtex.
Interventional radiologists Thomas Albrecht (Vivantes Clinic Neukölln, Berlin, Germany) and Roberto Iezzi (Policlinico Universitario Fondazione Agostino Gemelli, Rome, Italy) share their experience performing transarterial chemoembolization with degradable starch microspheres (DSM-TACE) using EmboCept S DSM 50 μm (Magle Group). Indicated for liver cancer treatment including hepatocellular carcinoma (HCC) and liver metastases from colorectal cancer (mCRC), and lung tumours, they detail how this invaluable “tool in [their] toolbox” has expanded effective options for interventionists to provide better patient care.
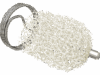
EmboCept S DSM 50 μm is an adjuvant in the intra-arterial treatment of inoperable liver and lung tumours in combination with cytostatic agents. Using microspheres of roughly 50 μm in size and with a half-life of approximately 35 minutes, EmboCept S DSM 50 μm can be used for super-selective treatments of single segments and selective targeting of one liver lobe to treat multifocal tumors.
EmboCept S DSM 50 μm in the landscape of TACE

EmboCept S DSM 50 μm DSM-TACE sits alongside drug-eluting bead transarterial chemoembolization (DEB-TACE), and conventional transarterial chemoembolization (cTACE), as a viable treatment option for patients with liver tumours. However, due to its unique degradable quality, EmboCept S DSM 50 μm can be used in a wider breadth of patients with varying levels of disease as Albrecht elaborates: “We use EmboCept S DSM 50 μm mainly in patients with multifocal or multisegmental disease, which is predominantly HCC in our practice, because you can treat patients with a high degree of efficacy and low toxicity.”
The degradable mechanism of action characteristic of EmboCept S DSM 50 μm allows for “transient” ischaemia, Albrecht states, detailing that this significantly decreases sides effects and improves the therapeutic effect. He adds that, during treatment, prolonged ischaemia has the potential to produce toxicity which can cause post-embolization syndrome and subsequently trigger loss of liver function. With EmboCept S DSM 50 μm however, the risk of these occurrences is “much less marked, if not minimal”, he says, providing a “much improved” safety profile, even when used in more extensive disease—“although we treat a larger proportion of the liver, it’s still better tolerated than other techniques”.
Treatment strategy

For Iezzi, the degradable characteristic of EmboCept S DSM 50 μm is also a notable benefit, enabling revascularisations “without concern over occlusion or collateralisation from a material point of view”. For mCRC, the ability to repeatedly perform treatment is key, as chemoembolization is often combined with irinotecan, which requires repeated activation by a healthy liver, he outlines.
“When providing care for mCRC, we need to apply a lobar approach, which involves a total of two treatments per lobe—or four treatments if it’s a bilobar procedure—performed with a delay of two to three weeks. It’s essential that we have the ability to perform repeated treatments within a very short period of time.”
In Iezzi’s view, the possibility to combine EmboCept S DSM 50 μm with various drugs, such as doxorubicin or epirubicin, which are also commonly used, is invaluable. “We are experiencing great results and its potential to be combined with other drugs [opens] the door for the treatment of new indications. Not only HCC or mCRC, but also cholangiocarcinoma and other liver metastasis, from pulmonary or gastrointestinal to gynaecological tumours,” he says.
“It’s a local treatment option for patients with advanced multifocal disease,” Albrecht states, expanding on the potential application of EmboCept S DSM 50 μm for a range of indications. “These patients would often not be treated with other types of TACE and they are being treated with radioembolization less often,” he says. Causing “minimal toxicity”, Albrecht conveys that EmboCept S DSM 50 μm is an “extremely well-tolerated” treatment option with very few side effects, making the procedure tolerable to patients at a wider range of disease level.
Evidenced clinical performance of EmboCept S DSM 50 μm
Informing their assertions, Iezzi and Albrecht worked side-by-side to conduct the largest retrospective European multicentre study, which scrutinised the safety and efficacy of DSM-TACE for advanced stage HCC in patients for whom were ineligible for other standard therapies or for whom these had failed . Their results were published in 2021 in the journal Cancers.
Led by Johannes M Ludwig (University Duisburg- Essen, Essen, Germany), the investigators identified 121 patients from three European centres. To be treated with DSM-TACE, patients were required to have had unresectable HCC with specific inclusion criteria between institutions. In Berlin, patients with a Barcelona Clinic Liver Cancer (BCLC) stage of C and D were deemed eligible; in Rome, patients with BCLC B refractory to TACE or stage C, those with a Child-Pugh class of A or B and those with an Eastern Cooperative Oncology Group (ECOG) status of between 0–1; in Essen, patients not suitable for ablation, transplantation, conventional TACE, radioembolization, or systemic therapy with kinase inhibitors, and an ECOG status of between 0–2.
They documented that the overall tumour burden in this population was high, with bilobar disease in 63.6%, >3 HCC nodules in 61.2%, and vascular invasion in 26.4%. Yet, their results showed that patients survived a median of 15.5 months with a median time of 9.5 months to tumour progression, and a 83.2% disease control rate. Additionally, they found that patients who survived longer had lesions of ≤10cm, the involvement of a single liver lobe, a lower Child-Pugh class and BCLC stage, and the absence of vascular invasion or of extrahepatic metastases.
In summary of their results, the investigators asserted that DSM-TACE using EmboCept S DSM 50 μm particles is a “veritable treatment option” for all unresectable HCC patients with high/diffuse tumour burden, “where other treatments fail or cannot be offered due to contraindications”.

The future of DSM-TACE with EmboCept S DSM 50 μm
For now, Albrecht says that he would like to see more interventionists using the technique, and to continue disseminating knowledge about its benefits to the wider community, with the approach still somewhat “unknown” in many countries. “For healthcare professionals, it’s an attractive option to be able to offer patients,” underlining how the effective treatment is also “relatively simple”.
Returning to the patient, Iezzi highlights that DSM-TACE using EmboCept S DSM 50 μm represents another treatment option for those in whom options may be limited. “It’s characterised by a high level of comfort for the patient,” he continues, “and it could be combined with a transradial approach”. In Iezzi’s belief, the demonstrable efficacy and safety of EmboCept S DSM 50 μm in liver tumours can “open the door” to future “outpatient and ambulatory care. The patient could be dismissed from hospital six hours after treatment” he adds, with the aim of offering effective and comfortable treatment options for patients.