Over the last two decades, the management of high-risk cirrhotic patients has developed significantly, with advances in pharmacologic, endoscopic and interventional radiologic treatment options. Since its introduction over a decade ago, the transjugular intrahepatic portosystemic shunt (TIPS) placement has become a fundamental treatment option.
Despite these advances, there still remains a high mortality rate of 20%–40% for high-risk variceal bleeders; and that is including the administration of rescue TIPS placements, said Dr Angelo Luca, Istituto Mediterraneo, Italy, at this year’s CIRSE meeting, Copenhagen, Denmark. Treatment failures are usually caused by repeated endoscopic therapy, multiple transfusions, frequent infections, and further liver deterioration, he added.
In a multi-centre, European randomised, controlled trial, Luca and colleagues evaluated whether an early decision to use TIPS with PTFE-coated stents in high-risk variceal bleeders improves the short- and long-term outcome as compared with the current recommended treatment using combined pharmacologic and endoscopic therapy.
Study design
In nine European centres, 63 high-risk cirrhotic patients with acute variceal bleeding (AVB), treated with vasoactive drugs and endoscopy, were randomised to receive PTFE-TIPS within the first 72 hours after admission (n=32) or to current recommended therapy (n=31). The primary endpoint was failure to control acute variceal bleeding and to prevent significant variceal rebleeding within in one year. Secondary endpoints included survival, development of hepatic encephalopathy, days in the intensive care unit (ICU), percentage of time of follow-up at the hospital, and the use of alternative treatments.
Patients included were those with liver cirrhosis, active bleeding from oesophageal or gastric varices, and Child-Pugh B plus active bleeding at endoscopy under pharmacological treatment or Child-Pugh C (<13). Patients excluded presented with hepatocellular carcinoma (HCC) beyond Milano Criteria, portal vein thrombosis, fundal or ectopic gastric variceal bleeding, or previous TIPS or drugs plus endoscopic therapy.
Results
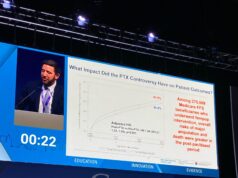
According to the results, 14 patients in the medical-endoscopic group vs. one patient in the PTFE-TIPS group reached the composite endpoint (p<.01). At one-year, actuarial probability of remaining free of the composite endpoint was 50% vs. 97% (p<.001), respectively.
Noteworthy, seven patients in the medical-endoscopic group received PTFE-TIPS as rescue therapy, and 16 patients died (12 in the medical-endoscopic group vs. four in the PTFE-TIPS group) (p<.02). One year actuarial survival was 60% vs. 86% in the medical-endoscopic and PTFE-TIPS groups, respectively (p<.01)
Luca added that one-year actuarial probability of new or worsening ascites were 33% vs. 13%, respectively (p=.11), and that of encephalopathy was 40% vs. 28% (not significant).
The complications observed included bleeding, severe infection, liver failure, Hepatorenal Syndrome, and arrhythmia, but were lower in the PTFE-TIPS group (Table 1).
Conclusions
“In high-risk cirrhotic patients admitted for acute variceal bleeding, early treatment with PTFE-TIPS is associated with marked reductions in rebleeding and mortality in comparison with the current gold standard therapy,” stated Luca. “Early treatment with PTFE-TIPS should be the treatment of choice in high-risk patients,” he concluded.