Attention should be focused on patients with iliofemoral and caval deep vein thrombosis and the balance should always be struck between the risk of bleeding and the long-term risk of post thrombotic syndrome, writes Stephen Black.
Attention should be focused on patients with iliofemoral and caval deep vein thrombosis and the balance should always be struck between the risk of bleeding and the long-term risk of post thrombotic syndrome, writes Stephen Black.
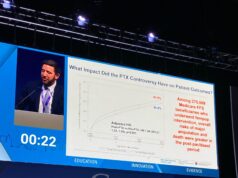
Interest in interventional treatment for deep vein thrombosis patients has increased exponentially in the last few years with the realisation that the current gold standard treatment (using elasticated compression stockings) may offer no effective treatment against progression to post thrombotic syndrome. In particular, the publication of randomised trial data (CaVenT, T Enden and colleagues, The Lancet, 2012) and meta-analysis supporting the use of lysis with contrasting studies suggesting that current management (as reported by the Sox trial investigators, Kahn SR and colleagues, The Lancet, 2014) does not work, has contributed to rising interest in interventional treatment. However, despite this enthusiasm, it is important to improve patient selection and techniques as well as to generate data to ensure that we treat patients appropriately and achieve long-term results.
The question of which patient are candidates for revascularisation needs to be evaluated by considering the following aspects.
Challenging age-old nomenclature
It is, after all, all in the name. The nomenclature of venous conditions needs re-examining. The definition of the anatomical location of deep vein thrombosis has for a number of years been based on the concept of proximal (ie, above the confluence of the calf veins to form the popliteal vein at the knee) and distal (ie, thrombosis below this anatomical location). This classification has therefore lumped a broad spectrum of heterogeneous patients into a single group. It is clear that the patients who will benefit the most (and are at the highest risk of post thrombotic syndrome) are those in whom clot involves the major vessels from the level of the groin up. It is imperative therefore that in considering patients suitable for treatment we, as practitioners understand that we should be treating the iliofemoral and caval systems, not femoropopliteal thrombus.
As De Maeaesneer and colleagues pointed out in the European Journal of Vascular and Endovascular Surgery in March 2016, the term “proximal deep vein thrombosis” is outdated and should not be used. A substantial effort on behalf of venous enthusiasts to standardise nomenclature and outcome measures is needed to fully clarify those patients who should receive lysis.
Balance of risk and benefits
The conflict of whether to use lytics or not has principally been a debate over whether patients were at greater risk from suffering bleeding complications than they were of developing post thrombotic syndrome and its consequences. Bleeding complications in the published trials, meta-anlaysis and single centre experience have been reassuringly low and the potential risk reduction for the development of post thrombotic syndrome may be significant. Techniques for delivering lytic have improved (as well as the development of non-lytic, purely mechanical, devices), potentially reducing bleeding risk. The major trials (CaVenT, CAVA and ATTRACT) have published exclusion and inclusion criteria which serve as the basis for most decision making. These criteria are understandably narrow. In our experience a considered discussion tailored to each patient, based on the age of clot, chance of success and risk of post thrombotic syndrome as well as a full engagement with the patient in decision making, is appropriate.
Improvement in patient selection
Increasing worldwide experience will likely result in improved patient selection. This will involve not just identifying patients in whom the thrombus will lyse, but also improved decision making with regard to patients who will and will not require a stent. It is well-recognised that history is an unreliable predictor of clot age and attempting to lyse thrombus that has already aged will not work. This practice exposed patients to the unnecessary risk of lytics for a poor chance of success. Improvements in determining clot age using MR techniques may well improve patient selection and help to rationalise treatment to only those with thrombus that is likely to lyse.
You need a team
At Guy’s and St Thomas’ Hospital in London, UK, we are blessed with an exceptional team of colleagues from vascular surgery, interventional radiology and haematology. There is no doubt that it is impossible to achieve good results without an exceptional team from nursing staff to clinicians who need to be fully educated in treating this disease because attention to detail is paramount.
Conclusion
The strategy of early clot removal is undoubtedly gathering momentum with the publication of several supportive papers and the eagerly awaited results from the randomised controlled ATTRACT trial. Attention should be focused on patients with iliofemoral and caval deep vein thrombosis and the balance should always be struck between the risk of bleeding and the long-term risk of post thrombotic syndome. Our focus should be on ensuring how we as a community gather robust, standardised data to demonstrate sustained long-term improvement in patient outcomes to justify the early enthusiasm for lysis.
Stephen Black is a consultant vascular surgeon and clinical lead for Venous and Lymphoedema Surgery, Guy’s and St Thomas’ Hospital, London, UK. He is a consultant to Cook Medical, Medtronic, Veniti, Volcano and Optimed.