Two-year data on the Passeo-18 Lux drug-coated balloon (DCB; Biotronik) continue to validate its safety and effectiveness in intra-inguinal arteries. Gunnar Tepe from the Klinikum Rosenheim in Germany presented 24-month results for the first time from the full cohort of the Passeo-18 Lux all-comers registry on behalf of the study group at the Leipzig Interventional Course (LINC; 22–25 January, Leipzig, Germany).
Tepe described the finding of 88.8% freedom from clinically-driven target lesion revascularisation (CD-TLR) as a “really good result in this challenging cohort”. The study also found 83.9% freedom from major adverse events, and 92.7% freedom from major target limb amputations with “a high number of patients which did not need to be amputated”. Despite a target lesion calcification rate of more than 76%, Tepe reported that only 15.7% of lesions treated required a stent.
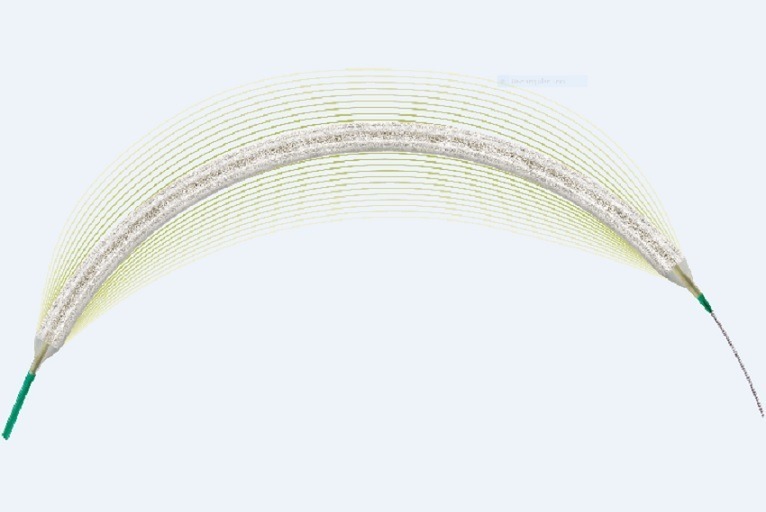
Biolux P-III is a prospective, global, multicentre all-comers trial of almost 900 patients to further investigate the Passeo-18 Lux DCB efficacy and safety in infra-inguinal arteries. It is conducted across 47 sites in 16 countries in the EU, Australia, and Asia. The DCB has a special excipient and comes with a safety guard insertion device which helps the drug to remain on the balloon, and prevents its loss on the sheath. Tepe described the study as the only real-world registry in infra-inguinal arteries, and it is the world’s second largest all-comers DCB registry.
Outcomes were freedom from major adverse events at six months, and freedom from CD-TLR at 12 months. Inclusion criteria were a lesion or lesions in the infra-inguinal arteries suitable for endovascular intervention treated with or scheduled to be treated with the DCB. Exclusion criteria were failure to successfully cross the target lesion with a guidewire. There were no patient or lesion characteristic limitations, and the use of additional devices was allowed.
“The special thing about the trial is that almost every patient could be enrolled, below-the-knee arteries as well as critical limb ischaemia (CLI) patients who may be excluded from other trials”, noted Tepe, with “42.1% CLI patients seen in the patient cohort and below-the-knee arteries were treated in almost 20% of the patients. In addition to that, [there were] high numbers of long lesions with C or D TASC classifications (32.6%), as well as a lot of patients with moderate to heavily calcified arteries (44.6%).”
Most patients were treated by pre-dilatation (72.3%, 784/1085), and the technical success rate was 98.4% (1068/1085).
At 24 months, the full cohort demonstrated 88.8% freedom from CD-TLR, “a very high number of freedom from TLRs”. Tepe suggested the large proportion of CLI patients in the study contributed to the major limb amputations rate. The mortality rate was 11.9%, with no increase over time, and the long-term rate remained the same at 180 days.
“We have to also acknowledge that there were a lot of patients enrolled in this study who have a higher likelihood to die—CLI over 40%, diabetes almost 50%, and patients being enrolled with previous cancer rates at almost 12%. This is not a prospective randomised trial comparing two percutaneous transluminal angioplasties (PTA) arms, so we cannot really compare to a control group, but what we can do is to look into mortality data and to look at one versus two years. There are not any major differences, nothing which strikes us and leads to the conclusion that this DCB is a risk or cause of mortality,” Tepe said.
The mortality rate among participants who are not CLI patients was lower: 2.9% (13/451) at 12 months and 5.5% (25/451) at 24 months. Other predictors of mortality were age, diabetes, and renal disease, and no significant differences in the distribution of cause of death between the first and second year were detected.
Feeding into the recent debate around paclitaxel use and late mortality, Tepe pointed out that dose of paclitaxel was not found to be a predictor of mortality in the Biolux P-III study. Although the low numbers within certain cohorts mean that dose dependency cannot be completely ruled out, Tepe observed “there are no signs that this drug-coated balloon is leading to mortality”, and concluded: “Biolux P-III … continues to confirm the safety and effectiveness of the Passeo-18 Lux DCB after 24 months.”
Tepe thus maintained that evaluated patient-level data showed no significant differences in the distribution of causes of death during the first year compared to the second year, and that no dose dependency of the mortality rate in the full cohort was observed.
CLI subgroup demonstrates low freedom from CD-TLR
Marianne Brodmann (Medical University of Graz, Austria) presented 24-month results from the largest CLI population enrolment in a real-world all-comer registry. Freedom from major target limb amputation was reported at 85.4%, and freedom from CD-TLR at 88.2%. The results also showed a crude mortality rate of 16.2% in the CLI subgroup.
Diabetes subgroup analysis reveals strong results in a challenging population
Focusing on a complex population of patients with diabetes, Johannes B Dahm (MVZ Herz- und Gefäßzentrum HGZ-Göttingen, Krankenhaus Neu Bethlehem, Göttingen, Germany) presented the results of 460 diabetic subjects from the registry with 53.1% CLI and 23.4% BTK lesions. In this subgroup, Dahm reported 87.5% freedom from CD-TLR and 87.4% freedom of major target limb amputation at two years.
Biotronik is extending the follow-up of paclitaxel-coated balloon studies to include long-term five-year patient data retrospectively on randomised control trials (Biolux P-I and P-II) and prospectively in the currently running all-comers registry, Biolux P-III.










