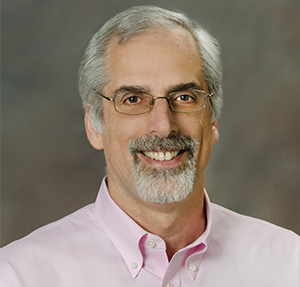
The Society of Interventional Radiology (SIR) has awarded John Kaufman with the Dr Charles T Dotter Lecture for his extraordinary career achievement and contributions to the specialty. The SIR has also given Gold Medals to Dimitrios Kelekis and Louis Martin for their contributions in advancing the quality of medicine and patient care. Interventional News spoke to them…
John Kaufman: Dr Charles T Dotter Lecture
John Kaufman has been chosen to deliver the 2012 Charles Dotter Lecture at the SIR annual meeting.
Kaufman is professor and Frederick S Keller endowed chair of interventional radiology at Dotter Interventional Institute and professor of radiology, professor of surgery and professor of medicine at Oregon Health and Sciences University, Portland, USA. He is also currently chief of vascular and interventional radiology and associate director of the Dotter Interventional Institute. In this interview, he told Interventional News the SIR award “Is a great personal and professional honour. I just hope that someone has not seriously misjudged me and that my lecture will not be too boring!”
A memorable clinical case
“The cases that stand out in memory are not always the most dramatic or heroic. If I had to pick one, it would be a current patient; an 18-year-old with very bulky primary hepatoma (not fibrolamellar). The patient has absolutely no risk factors, which lead to a significant delay in diagnosis. We are slowly working through multiple liver directed therapies, and getting a good response in terms of imaging and symptoms. But what really stands out is this young person’s courage and resolve to be a normal 18-year-old in the face of something so inexplicably unfair as hepatoma. We need to remember always that we treat patients, not lesions or diseases.”
Key moments for interventional radiology
“The first was when Charles Dotter dilated an artery in 1964—this created an entirely new and fundamental approach to patient care, the use of imaging to guide intervention rather than just make a diagnosis. I do not have a date for the next critical moment, but it was when cardiology replaced radiology as provider of cardiac catheterisation, a clear signal (that has been repeated many times) that technical expertise is not enough to maintain a role in the procedures that we develop. And of course 1994, when the American Board of Radiology awarded the first subspecialty certificates in vascular and interventional radiology, formalising recognition of interventional radiology by all of the other boards in medicine.”
Most importantly…
“We must be able to show that SIR president (2011—2012) Tim Murphy’s summation of interventional radiology as ‘faster, safer, better, cheaper’ is actually true.”
Message to peers
“We have one of the best jobs in medicine with a great future; let us work to keep it that way.”
The 2012 Charles T Dotter Lecture will be delivered Monday, 26 March
Dimitrios Kelekis: SIR‰ÛöGold Medal
Born on 19 August, 1938 in Thessaloniki, Macedonia, Greece, Dimitrios Kelekis is the first interventional radiologist in a family of three generations of radiologists. Widely regarded as a pioneer of interventional radiology in Greece, he has served as president of the Hellenic Society of Interventional Radiology, Vascular Radiology and Neuroradiology for many years and is respected as a teacher to many generations of interventional radiologists. Kelekis was professor of Radiology, University of Athens, Greece, president of the CIRSE annual meeting in 1994 in Crete, and will be awarded the SIR Gold Medal in 2012.
Kelekis was influenced by family members who were doctors from a very young age. His father, uncle and cousins were all doctors, and all his immediate family including his father were radiologists. Even his godparent at his baptism was an eminent radiologist! Kelekis said: “I belong to a family of radiologists and we took part in discussions on barium examinations from childhood. I was naturally drawn to radiology when I studied it in my medical school years.”
Teachers and influences
Kelekis recalls, “Philippe Bussat was my first teacher in angiography in 1968. I was also influenced and impressed by the work of Anders Lunderquist, Erik Boisen and Erikson. A very important influence was the Paris School with Hernandez and Escoffier, as also Professor Zeitler. He also had the joy of working with Andreas Gruentzig. “I had the privilege to meet and work with Andreas Gruentzig, from whom I learnt percutaneous transluminal angioplasty. Christos Athanasoulis and his team in MGH were fundamental to my evolution as an ‘interventionalist’.”
Why interventional radiology?
“During my residence in Geneva I was impressed by the potential of interventional radiology, and it was more suitable to my active character,” said Kelekis. Now his son, Alexis Kelekis, his daughter-in-law and two nephews (plus their families) are part of a family of six active radiologists who provide the third generation of imagers and second generation of interventional radiologists
Major milestones
- First selective coronographies in Greece (1970)
- First selective angiographies in Greece of renals and splanchnic arteries (1970–1971)
- First studies of women’s venous system in Greece (1973)
- First transthoracic lung biopsies in Greece (1975)
- Pharmacodynamic studies of different drugs in superior mesenteric artery in dogs
- First percutaneous transluminal angioplasty in Greece (1980)
- First embolization in Greece (1982)
- First publication in Greece on recanalisation of tubes
- Stent placement in aortic aneurysms (more than 100 cases)
The SIR‰ÛöGold Medals will be awarded on Tuesday, 27 March
Louis Martin: SIR‰ÛöGold Medal
Journey into interventional radiology
“My father wanted to be a doctor but he graduated from high school during the Depression and could not go to college. He never pressured me to go into medicine, but I knew it would make him very happy if I did, so every time I had an academic choice to make I just kept gravitating in that direction.
Three important points for a teacher of interventional radiology…
- It is an honour and privilege to be allowed to treat a patient. It is our duty to make sure that the treatment is appropriate and performed to the very best of our ability. The patient and their family must be treated with the care and consideration that you would wish for yourself or a loved family member. It is important that they meet the operator before the procedure and are personally informed of the results after it.
- Be honest with the patient and yourself.
- Do not be afraid to ask questions. Search for alternate answers. Be skeptical of those who know the ‘right’ answer, there is frequently more than one.
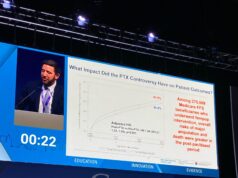
Measurement of complications
I think we do very poorly in evaluating our complications to interventional procedures.
Unless we are working under a very strict research protocol, the tendency is to explain away or divert the blame for procedural complications. This is human nature and it is true that the causes of the complications are frequently multifactorial. I think that a major problem is using the word “complication”. It is confrontational and pejorative and immediately places the operator in a defensive position. I think it is much better to use the term ‘adverse event’ which does not inherently assess blame or quantify the event. For example: it is not unusual to incite a transient arrhythmia while placing a central venous line. Is it a complication? Do we really know? The arrhythmia rarely requires medication or electrical conversion and is usually not recorded in the post-procedural dictation. It is therefore impossible to retrospectively investigate the incidence, mitigating factors or importance of this event. Transient, seemingly unimportant events such as an arrhythmia, hypoxia, hypoglycemia, elevation or reduction in body temperature, leukocytosis or change in the basic metabolic profile go unrecorded unless they progress into an event that requires a major change in patient treatment. I think adverse events occurring during or after an interventional procedure should be rigorously recorded so that we can use this knowledge to improve patient care.”