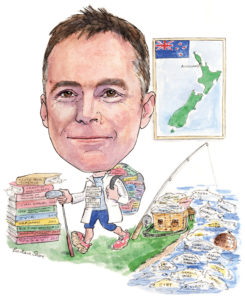
 “If you are clinically skilled, achieve a high level of technical training in interventional radiology procedures, have the best audited results for a procedure and a good relationship with your clinical colleagues, you are always going to be busy and have a highly successful career,” Andrew Holden, convenor, Central Organising Committee Members, Asia Pacific Society of Cardiovascular and Interventional Radiology (APSCVIR) tells Interventional News. Holden is director of Interventional Radiology, Auckland Regional Public Health Service, and associate professor, Radiology, at Auckland University School of Medicine, Auckland, New Zealand.
“If you are clinically skilled, achieve a high level of technical training in interventional radiology procedures, have the best audited results for a procedure and a good relationship with your clinical colleagues, you are always going to be busy and have a highly successful career,” Andrew Holden, convenor, Central Organising Committee Members, Asia Pacific Society of Cardiovascular and Interventional Radiology (APSCVIR) tells Interventional News. Holden is director of Interventional Radiology, Auckland Regional Public Health Service, and associate professor, Radiology, at Auckland University School of Medicine, Auckland, New Zealand.
What made you choose interventional radiology? What still motivates you in this field?
When I was a junior hospital doctor, I was attracted to radiology because it was a dynamic and rapidly changing specialty. However, I missed direct patient contact and the rewards associated with managing patient problems. Image-guided intervention (or interventional radiology) provided me with great opportunities to combine evolving technology with minimally invasive therapy. The rate of progress has not slowed and continues to challenge and stimulate me.
Who were your mentors and what wisdom did they impart to you?
Everyone has role models and for me two international pioneers who influenced my career (and still do) were Barry Katzen (Miami, USA) and Michael Dake (Stanford, USA). Both interventional radiologists gave me an early understanding of the value of being clinically relevant and contributing to a multidisciplinary approach. Locally, my recently-retired colleague, Alan List, taught me the importance of respecting your patients and colleagues as well as keeping humour in your day.
Which innovation in interventional radiology has most influenced your career?
Without doubt, endoluminal repair of aortic aneurysm disease has had the most profound influence on my career. By good luck rather than good management, I was involved in the first bifurcated endovascular aneurysm repair (EVAR) devices with Michael Lawrence-Brown and David Hartley at Royal Perth Hospital, pioneering a device that would become the Cook TriFlex device. Subsequently, I have had the privilege of being involved in many EVAR “first-in-human” and live case presentations as this technology continues to develop.
The most important change in the last decade has been the development of a quality vascular research programme at Auckland Hospital. We have been involved in over 30 first-in-human device trials over that period as well as multiple multicentre trials and registries. Traditionally, interventional radiology has not been as strong as other specialties in participating in clinical trials that support evidence based practice, but this is changing.
In the new age of big data healthcare, personalised medicine, robotics and specialties coalescing and separating, can you please describe the future of image-guided interventions as you see it?
The future of image-guided, minimally invasive intervention has never looked brighter. The ability to perform procedures under fused or virtual imaging control with the associated reduction in patient and staff radiation is already established and will continue to evolve. Technological advances will facilitate more refined and new procedures. Interventional oncology, in particular, is an area of huge growth potential. In terms of specialties coalescing, I have always taken the approach that the patient benefits most when the skill sets of physicians are combined.
As an interventional radiologist who is at the forefront of vascular interventional practice, how will the development of the endovascular specialist affect the “interventional radiologist” who wants to maintain a thriving endovascular practice?
I believe interventional radiology must embrace the concept of an endovascular specialist. For example, at Auckland Hospital, our interventional radiology fellows are encouraged to spend time in vascular surgery, acquiring relatively simple surgical skills as well as attending outpatient clinics. The vascular surgical fellows also spend time in the interventional radiology suites. The hybrid operating room provides a unique opportunity for multidisciplinary interaction. The distribution of workload should ultimately be decided by the skill set and outcome audit, rather than the specialty background. While most proceduralists perform simple interventions well, the ability to perform complex interventions with excellent outcomes is much more limited. This is particularly true in critical limb ischaemia, where the endovascular specialist must be able to demonstrate high levels of success with crossing chronic total occlusions, retrograde access, etc. My advice to the interventional radiologist who wants to maintain a thriving endovascular practice is to offer a clinical and procedural service, achieve superb technical skills and collect and publish outcomes. If you are clinically skilled, achieve a high level of technical training in interventional radiology procedures, have the best audited results for a procedure and a good relationship with your clinical colleagues, you are always going to be busy and have a highly successful career.
Could you briefly describe how interventional radiology is practised “down under” and in the wider Asia Pacific region?
Throughout the region, interventional oncology procedures are almost entirely performed by interventional radiologists. This will continue to grow, supported by trial evidence and new procedures. Venous intervention is also growing, as is interventional neuroradiology, particularly with the development of acute stroke services in many centres. Like most parts of the world, there are geographic variations in who performs endovascular procedures with interventional radiology playing a major role in many countries in the Asia Pacific.
What are your key goals as the convenor of the upcoming APSCVIR meeting in March 2018 in Auckland?
The APSCVIR is our regional interventional radiology society similar to CIRSE in Europe and SIR in North America. APSCVIR is rapidly developing and has enormous potential, particularly as there are more interventional radiologists practising in the region than any other region globally. APSCVIR 2018 (apscvir2018.com) aims to bring together a superb international and Asia Pacific faculty to discuss the latest developments, focusing on endovascular and interventional oncology topics. Live cases, multidisciplinary discussion forums and many visiting societies should contribute to an excellent learning opportunity. Late summer is also a great time to visit Auckland and New Zealand!
What clinical science are you most excited about showcasing at the APSCVIR meeting?
These are exciting times for interventional radiology with many recent trial results and device developments becoming available. At APSCVIR 2018, we intend to present and debate these results in attempt to provide some consensus on optimum current treatment strategies.
How has research changed in interventional radiology? What do you make of the recent high-profile trials such as ATTRACT and SIRFLOX that have not shown a benefit for interventional radiology procedures?
Quality research has greatly improved and increased over the last decade. It is very important for interventions to be supported by a solid evidence base, particularly in the current cost-conscious environment. The ATTRACT trial is a good recent example and provides evidence-based support for iliofemoral revascularisation in chronic venous insufficiency but not revascularisation below the inguinal ligament. This facilitates clear and consistent decision making. Likewise, recently presented trial data evaluating the role of radioembolization in the management of hepatocellular carcinoma (SARAH/SIRveNIb) and colorectal metastatic disease (SIRFLOX/FOXFIRE) have contributed significantly to understanding how this therapy fits in to the oncology armamentarium.
Which of the trials that you are involved in currently are you most looking forward to the results of?
We are currently involved in over 25 vascular device trials in various stages of recruitment and follow-up. Lower limb arterial trials include drug-coated balloon trials (with devices such as Stellarex [Spectranetics] and Ranger drug-coated balloon [Boston Scientific]) and drug eluting stent trials such as XPEDITE (Cook Medical) and MAJESTIC (Boston Scientific). I am looking forward to the results of the IMPERIAL trial that will provide a head-to-head comparison between two different drug-eluting stent platforms. We are currently involved in a number of trials that embrace different methods of angioplasty and vessel preparation. Shockwave lithoplasty is a fascinating example of this (we are currently recruiting to DISRUPT PAD III) but we are also involved in trials using the Trireme Chocolate drug-coated balloon and the Cagent Serranator device. Bioresorbable scaffolds have been challenging, but we are currently recruiting to the Elixir DESappear trial. On the aneurysm front, we performed the first-in-human experience with the Ovation Alto platform and are involved in the Endologix Nellix FORWARD 2 registry. Other trials we are currently involved in include several embolization and venous device trials. I am lucky enough to be one of the principal investigators in the Medtronic drug-coated balloon in arteriovenous access randomised trial that I hope will support an important advance in dialysis access intervention. Finally, I do hope that the COROLLARY trial gets underway. This is a trial proposed by the CORAL trial investigators who noted that patients with low baseline albuminuria did significantly better with renal artery revascularisation than those treated medically. It may be that albuminuria is the biomarker we have been looking for to assist in selecting patients who will benefit from renal artery revascularisation.
Which early technologies in interventional radiology are you keeping an eye on?
In the peripheral vascular space, the advent of drug-eluting technologies has improved patency but primarily in short to medium length, relatively simple, lesions. The concept of adequate vessel preparation is expanding to allow more complex disease to be successfully treated with these therapies. Many devices that may be considered standalone or vessel preparation devices are currently being evaluated including the Shockwave Lithoplasty system for heavily calcified lesions and the Cagent Serranator device.
In the aortic space, I have long believed that active aneurysm sac management is the key to providing a durable outcome with minimal reintervention. Aneurysm sac filling technologies, either as part of the primary endoluminal device (eg Endologix Nellix) or as an ancillary to conventional EVAR (eg Arsenal Medical) remain of great interest. There are also many technological and procedural innovations in both venous intervention and interventional oncology.
What have been the biggest challenges for interventional radiology in 2017?
As the indications for minimally invasive, image-guided therapy continue to expand, the need for well-trained physicians with excellent procedural and clinical skills also grows. This is the biggest challenge for interventional radiology. It is not surprising that the junior membership of interventional radiology societies such as SIR and CIRSE is at record levels but this must continue if image-guided therapy is to reach its potential.
Could you describe a memorable case?
There are many I could describe but one was a live case broadcast to a European meeting. I was performing the case late in the evening in New Zealand to facilitate time differences. It was a tricky, large main renal artery aneurysm that I was treating with a self-expanding covered stent. The case went very well but was complicated by guidewire induced spasm so I was giving repeated boluses of intra-arterial vasodilator. At the end of the procedure, I was congratulated by the live case panel and could hear the applause from 10,000 kilometres away. Thirty seconds after the live transmission ended, the controlled environment of the interventional radiology theatre turned upside down as the patient collapsed and was unresponsive. Fortunately, it was only a vaso-vagal induced hypotensive episode, probably exacerbated by the vasodilators, and the patient fully recovered. However, it reminded me of the challenges and sometimes good fortune needed to perform live cases.

What are your interests outside of medicine?
I have a great family and enjoy spending time with them. We have a beach house and enjoy water sports there—swimming, fishing, snorkelling, etc. I like to keep fit with cycling and running and enjoy most sports although, like most New Zealanders, rugby is a passion.













