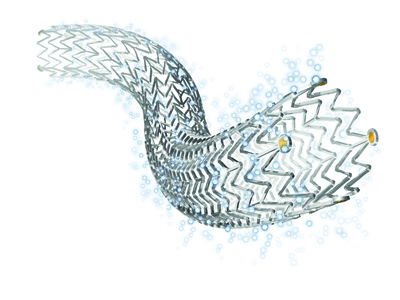
Preliminary results of a randomised controlled trial comparing the use of the Zilver PTX drug-eluting stent (Cook Medical) and bypass grafts in long femoropopliteal lesions show a trend in favour of the endovascular device at 12 months with lower rates of restenosis and target lesion revascularisation. Initial results of the ZILVERPASS study were presented at the Leipzig Interventional Course (LINC; 26–29 January 2016, Leipzig, Germany).
Marc Bosiers, head of the Department of Vascular Surgery, St Blasius Hospital, Dendermonde, Belgium, noted that bypass surgery is the gold standard for TASC C and D femoropopliteal lesions. “If we look at the results published in the last few years for ePTFE and Dacron grafts, we can see that the average primary patency at one year is 78%,” he said.
He explained that there is a difference in the assessment of patency in open surgery and endovascular surgery, with endovascular intervention assessing the absence of primary binary stenosis (PSV≥2.4) and open surgery assessing whether the vessel is “open or closed”. Bosiers said that in order “to compare apples with apples”, his group investigated 100 bypass procedures that were surgically revascularised at his institution and assessed if those bypasses presented with binary stenosis, either at the proximal or distal anastomosis, for example. He continued, “We found that 11 of those bypasses, in the endovascular world, would have been qualified as having lost primary patency. This would bring the primary patency of a bypass, in the endovascular world, to around 70%.”
A subanalysis of the ZILVER PTX trial looking at 135 long lesions (TASC C and D, average lesion length 23cm) treated with the device showed a primary patency rate of 77.6% and a freedom from target lesion revascularisation rate of 85%. “Comparing this with the bypass performance, with a primary patency of 70% or 80%, depending on the way you look at it, we were able to convince Cook Medical to support a randomised controlled trial of bypass vs. Zilver PTX,” Bosiers told delegates.
ZILVERPASS (The Cook Zilver PTX drug-eluting stent versus bypass surgery for the treatment of femoropopliteal TASC C & D lesions) is a prospective, multicentre study and will randomised 220 patients in a 1:1 fashion in Belgium, Brazil, Germany and Italy.
Bosiers presented preliminary data on the first 114 patients enrolled in the study. The inclusion criteria were patients presenting with lifestyle-limiting claudication, rest pain or minor tissue loss (Rutherford category 2–5), stenotic or occlusive de novo lesion located in the femoropopliteal arteries, suitable for endovascular therapy and bypass surgery, and total target lesion length of at least 150mm. Patients with previous surgery and/or endovascular procedure in the target vessel were excluded.
In both study arms primary patency at 12 months was defined as absence of binary restenosis or occlusion within treated lesion and absence of target lesion revascularisation within 12 months.
There was no difference between the two arms in terms of Rutherford classification. The duration of the procedure was significantly lower in the Zilver PTX group compared to the bypass group (58.67±39.72min vs. 103.25±42.74, p<0.001), and the lesion length in the Zilver PTX arm was lower than in the bypass arm (239.11±63.67mm vs. 267.07±76.3mm, p=0.036).
For the first 114 patients, the Kaplan Meier analysis showed that primary patency at 12 months was 78.1% with Zilver PTX and 68.7% with bypass surgery, p=0.550, “a trend in favour of Zilver PTX” according to Bosiers. “You may think this is low for bypass, but I must emphasise that this looks at binary stenosis at the proximal or distal anastomosis. But even if you look at freedom from target lesion revascularisation, you see that this is 75% vs. almost 90% in the Zilver PTX arm. These are very promising results but we will need to wait for the full enrolment and final data to see who wins this match.”
The ZILVERPASS study is estimated to be completed in November 2017.











