Percutaneous vertebroplasty does not result in statistically significant greater pain relief than a sham procedure, reports a study detailing the results of the VERTOS IV trial, published in the British Medical Journal (BMJ). This study followed patients with acute osteoporotic vertebral compression fractures for 12 months following either a vertebroplasty or a sham intervention.
After the 2009 masked randomised controlled trials published in the New England Journal of Medicine, INVEST (Kallmes et al) and the Australian trial (Buchbinder et al), both found no benefit for vertebroplasty over a sham control, there was an angry backlash from interventionalists who questioned both the trial designs and their findings.
Kallmes, who repeatedly clarified that in the INVEST trial, vertebroplasty worked, just not significantly better than the sham intervention (which also, for some reason, had worked rather well) went on to publically declare himself likely “the most reviled radiologist on the planet”.
A potential upshot of these trials, according to prevailing community opinion, was that vertebroplasty began to be eyed with caution in some quarters and the numbers of these cement augmentation procedure began to dwindle. Then came the results of the 2010 open-label VERTOS II (Klazen et al, The Lancet) and the 2016 masked Australian VAPOUR trial (Clark et al), the results of which gave vertebroplasty a much-needed boost. Many interventionalists felt vindicated that their observations of vertebroplasty ‘done right’ i.e., in acute vertebral compression fractures and using an adequate volume of cement, were finally being borne out. And yet, here are the results of the VERTOS IV group (Firanescu et al) whose data follow the path of the 2009 trials. The question is: what does this mean for the continued clinical role of vertebroplasty?
Patient selection
VERTOS IV is a blinded, sham controlled clinical trial that included 176 patients: 90 participants, with 115 fractures, in the vertebroplasty group and 86 participants, with 108 fractures, in the sham procedure group. Patients referred to four radiology centres for spinal radiographs who were found to have radiographic fractures were administered a questionnaire. Those with a VAS pain score of at least five out of 10 and duration of fracture less han nine weeks were invited to enroll.
Consenting patients were referred for MRI and physician consult and if still deemed eligible underwent the procedure 11 to 13 days later (mean 6.1 weeks). This was an outpatient only trial.
The procedures
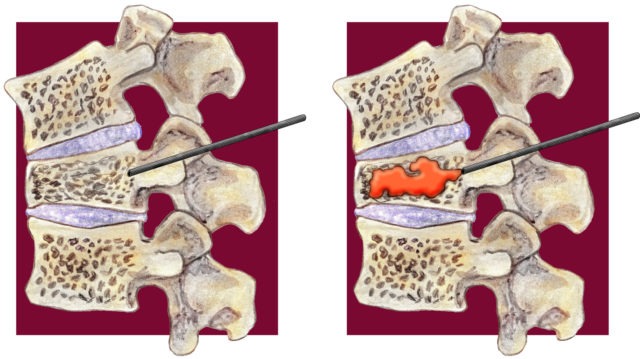
All participants received local infiltration with 1% lidocaine (lignocaine) into each pedicle followed by 0.25% bupivacaine.
Next, each participant received two stab incisions at the level of the vertebral body, after which the sealed randomisation envelope was opened—the patient was then assigned to either the vertebroplasty or the sham group.
For both groups, the cement was prepared in close proximity to the patients, who could hear the mixing sound and smell the PMMA in the room. However, while the cement was injected in the vertebroplasty group, the injection was simulated in the sham procedure group using verbal and physical cues. Bone biopsy needles were positioned bilaterally, with the sham intervention involving periosteal placements instead of transpedicular placements. After the procedure, participants in the vertebroplasty group underwent computed tomography, whereas participants in the sham procedure group were subjected to preliminary scout view scanning only.
Findings
First author Cristina E Firanescu (Departments of Radiology and Internal Medicine, Elisabeth TweeSteden Hospital, Tilburg, The Netherlands) and colleagues report that compared with baseline, the reduction in the visual analogue scale (VAS) score over 12 months in both groups was clinically and statistically significant at all measurement points: one day, one week, and one, three, six and 12 months. Firanescu et al write, “This significant reduction was measurable starting at day one after the procedure and remained significant throughout the follow-up.”
The primary prespecified objective of the VERTOS IV trial was to determine the difference between groups in mean reduction of VAS score during 12 months’ follow-up, at one day, one week, and one, three, six, and 12 months after the procedure. The VAS score ranged from 0 (no pain) to 10 (severe pain).
Quality of life improved for both the vertebroplasty and the sham procedure groups. The quality of life questionnaire of the European Foundation for Osteoporosis (QUALEFFO) and physical functioning with the modified Roland-Morris disability (RMDQ) questionnaire scores were used as secondary endpoints of the study.
For both measures, the worse the health related quality of life condition, the higher the score. There was a statistically significant decrease in both the QUALEFFO and RMDQ scores compared to baseline at all time-points measured during the 12 months’ follow-up period.
The mean reduction in QUALEFFO score at the last measurement point (12 months) was 18.32 in the vertebroplasty group (95% confidence interval 18.32 to 23.61) and 18.61 in the sham procedure group (13.02 to 24.2), with a between group difference of −0.14 (95% confidence interval −3.04 to 2.76). The mean reduction in RMDQ score at the last measurement point (12 months) was 7.71 in the vertebroplasty group (5.87 to 9.55) and 7.47 in the sham procedure group (5.56 to 9.38), with a between group difference of 0.12 (−1.11 to 1.35).
The study authors hypothesise, “These results suggest that factors aside from instillation of PMMA might have accounted for the observed clinical improvement after vertebroplasty; for example, the effect of local anaesthesia, expectations of pain relief (placebo effect), natural healing of the fracture, and regression to the mean.”
Speaking to Interventional News, Firanescu pointed to one way of looking at these findings: “Although percutaneous vertebroplasty did not result in statistically significantly greater pain relief than a sham procedure, more patients show secondary fractures and persistent pain in the sham group. A future therapeutic pain strategy could be a combined regimen of periosteal infiltration during natural healing. Additional cement seems indicated only in a selected subgroup of patients with insufficient pain relief after this early phase,” she says.
Recent history of blinded trial evidence
The Kallmes et al and Buchbinder et al trials in 2009, two blinded randomised studies, found no benefit of vertebroplasty compared with sham controls. The VAPOUR (Vertebroplasty for Acute Ppainful osteoporotic fractURes) trial showed that better pain relief was achieved after vertebroplasty compared with sham treatment, as measured by a clinically significant pain reduction at all time points from three days till six months, with the primary endpoint at 14 days. There was also significant reduction in disability, improved quality of life and 30% greater preservation of vertebral body height.
David Kallmes (Mayo Clinic, Rochester, USA), principal investigator of the INVEST trial, tells Interventional News: “Aiming to ‘correct’ numerous apparent deficiencies in patient selection criteria in prior blinded augmentation trials, the VERTOS IV investigators have instead joined those casting doubt on the technique. Notably, the results of VERTOS IV, in which 75% of patients were treated beyond 28 days, are in fact entirely congruent with those of the VAPOUR trial, which demonstrated that fractures three weeks of age and older did not benefit from spine augmentation. If the VERTOS family of trials, with unblinded VERTOS II showing profound comparative benefit of the cement that vanished with blinding in VERTOS IV, has shown us anything it is that effective blinding in spine augmentation trials is essential. VERTOS IV provides additional concrete evidence that the spine augmentation procedure reduces pain and improves function and quality of life, but we must continue to try to understand why some patients experience these benefits without cement.”
Of the contrasting results between the most recent VERTOS IV trial and the VAPOUR trial, William Clark (Department of Radiology, St George Private Hospital, Kogarah, Australia), principal investigator of the 2016 VAPOUR trial, comments, “VAPOUR and VERTOS IV are very different trials. The VAPOUR trial used different patient selection criteria to VERTOS IV, with earlier vertebroplasty (2.8 weeks vs. 6.1 weeks mean pain duration). VAPOUR included hospitalised inpatients and outpatients with severe (NRS≥7/10) pain despite analgesic therapy (including opiates in 90%) and offered vertebroplasty without further delay. VERTOS IV was outpatient only, 34% of patients were taking strong opiates, VAS pain threshold was 5/10 and there was 13-day delay between initial recruitment and vertebroplasty. The benefits of vertebroplasty in VAPOUR were concentrated in patients with fractures ≤ 3 weeks duration, with no advantage over placebo in fractures greater than three weeks. At the time of vertebroplasty 88% of patients in VAPOUR had fractures less than or equal to four weeks duration compared to 25% in VERTOS IV. These differences explain the different trial outcomes. Vertebroplasty should be reserved for patients (including inpatients) with severe, uncontrolled pain despite maximal medical therapy and should be offered early, without undue delay.”
Afshin Gangi (Radiology and Nuclear Medicine, Imagerie Interventionnelle, Strasbourg, France; Oncological Interventional Radiology, King’s College London, Guy’s and St Thomas’ NHS, London, UK) concurs with Clark, saying, “Patient selection is really the key… [this trial is] treating patients too late—we need to treat them faster to reduce the immobilisation and stop spinal deformation and hyperkyphosis. Vertebroplasty stops vertebral collapse and avoids the eventual progression to spinal deformation. They [the VERTOS IV trial investigators] just evaluate the pain.”
Commenting on the importance of the data, Joshua Hirsch, vice chair of Interventional Radiology, service line chief, Interventional Radiology, director, Interventional Neuroradiology, chief, NeuroInterventional Spine, Massachusetts General Hospital, Boston, USA and Harvard Medical School, Boston, who is a coauthor of VERTOS IV, says: “We believe VERTOS IV to be an important addition to the existing augmentation literature. While this trial suggests that there may be a role for the use of high volume periosteal anaesthetic in vertebral compression fracture patients, this approach would require further validation through open label trials. Moreover, it is critical to appreciate that the real-world alternative to augmentation for compression fractures is conservative therapy. Such treatment including opiates, limitation of activities of daily living and bedrest have their own risk profile. Vertebral augmentation results in early mobilisation and sagittal preservation. These are likely important factors leading to the strong evidence for morbidity and mortality benefits associated with augmentation. It is our sincere hope that the results of VERTOS IV are carefully scrutinised leading to thoughtful interpretation and conclusions.”