Clinicians based at the Royal Stoke University Hospital (Stoke-on-Trent, UK) have developed a new protocol for uterine fibroid embolization (UFE), introducing a day case service option for these patients. Despite a body of opinion convinced that the immediate post-procedural phase is too painful to treat UFE patients on an ambulatory care basis, the study investigators report a near perfect success rate in the small initial patient cohort discharged on the same day as embolization.
Of the first ten patients to follow the new Stoke protocol, nine were discharged before 8pm and had no complications after 48 hours, as determined by a nurse-led follow-up phone call. One patient did progress to an overnight stay, but this was due not to any pain or complications, but to the fact that she had failed to disclose that there would be no adults at home to care for her overnight, a prerequisite of same day release from hospital.
David Wells (University Hospitals of North Midlands NHS Trust, Royal Stoke University Hospital, Stoke, UK) and co-authors conclude: “Using a collaborative, evidence-based approach, tailored to the specific needs of patients undergoing UFE, we were able to formulate a safe, effective and validated strategy for a day case procedure. We do expect some patients to be re-admitted for pain control. This should not be seen as a failure of day case, [but] rather a safety net for some patients.”
In a healthcare system under the strain of in-patient bed shortages, Wells and colleagues decided to review standard practice in order to “find ways of delivering effective therapy to patients in more efficient ways.” They worked with patients, anaesthetists, gynaecologists, and day case and surgical assessment units to provide women with the option of a day case procedure.
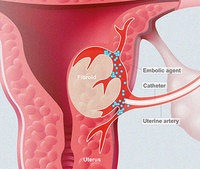
The adoption of a trans-radial arterial approach was crucial in facilitating this conversion of UFE treatment to a day case procedure for the Stoke team. Compared with a trans-femoral approach, Wells and colleagues found trans-radial access to dramatically reduce the risk of significant access site haemorrhages, and the approach allowed patients to mobilise immediately.
Describing their methods, the authors comment: “Closure of the radial arteriotomy is achieved using a variable compression wrist device. Once this radial band is removed (which takes on average 40 minutes) and the discharge protocol parameters met, the patient can be safely discharged. The only issue to manage then is pain.”
In 2017, the then current day case analgesia practices for patients undergoing gynaecological day case surgery were reviewed. Prior to revision, the strategy for managing patient’s ischaemic pain from embolizing the uterine arteries at the Royal Stoke University Hospital relied on preoperative anti-inflammatory medications and patient controlled anaesthesia during the procedure and overnight stay. However, patient controlled anaesthesia resulted in a significant number of patients with opioid related nausea and constipation—these were the main complaints seen in follow-up. Delays in taking down the patient controlled anaesthesia set-up led to significant discharge postponement for patients following an overnight stay.
Therefore, the study investigators researched other strategies for pain relief. They found that, given preoperatively, gabapentinoids provide anxiolysis for patients, and the authors cite evidence that this class of drugs significantly reduces opioid consumption in the postoperative period.
The authors give a detailed description of the development of this day case service, as well as the pain relief regimen and its rationale, in an article published in the New Journal of One Day Surgery.










