
The PErFecTED technique stands for Proximal Embolization First, Then, Embolize Distal for benign prostatic hyperplasia, writes Francesco Carnevale, São Paulo, Brazil. He will receive the CIRSE 2016 Award of Excellence and Innovation in Interventional Radiology. The award is sponsored by the R Guenther Foundation and seeks to reward and encourage exceptional research in the field of interventional radiology.
Prostatic artery embolization is an important alternative treatment for patients with lower urinary tract symptoms due to benign prostatic hyperplasia. A refined embolization technique is crucial for imaging and clinical success. With over eight years of follow-up, we have amassed significant clinical and technical experience and believe we should share these technical improvements that we have learnt with others.
With this technique, pelvic angiography is first performed to evaluate the iliac vessels and the prostate arteries. This helps us to better understand the anatomy, identify any atherosclerotic problems and choose the best technical strategy. A selective digital subtraction arteriogram of the internal iliac artery with a 5F cobra or vertebral diagnostic catheter placed at the common internal iliac trunk is performed to assess the blood supply to the prostate and perform the inferior vesical artery catheterisation under ipsilateral 25–55 degree oblique view. For the ipsilateral internal iliac artery approach, the Simmons or the vertebral and cobra catheters with a Waltman loop can be used.
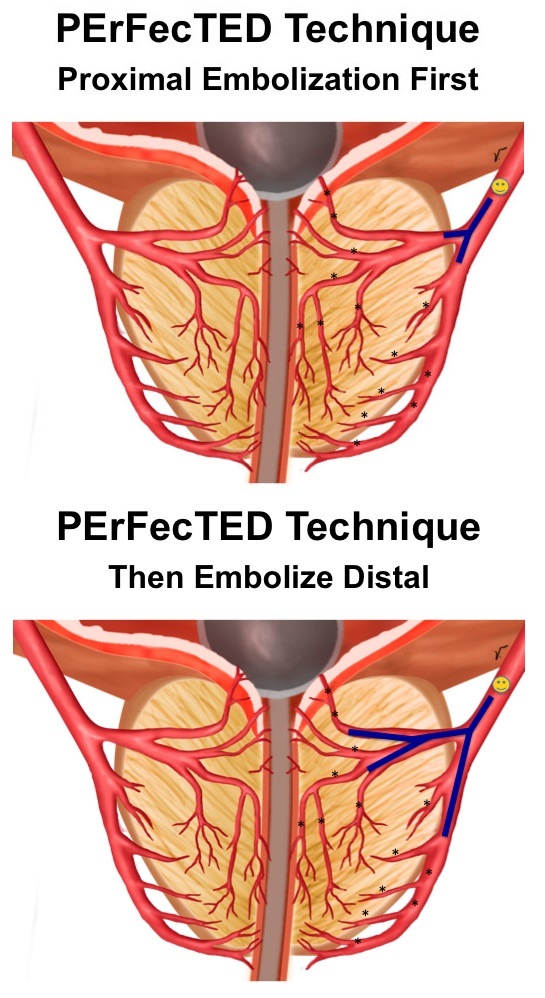
Proximal Embolization First (Figure 1A)
After entering the inferior vesical artery, a vasodilator (nitroglycerine or isosorbide mononitrate) is injected through the microcatheter to prevent vasospasm, and increase the artery size to facilitate microcatheter navigation and distal positioning. The microcatheter should cross any collateral branch to the bladder, rectum, corpus cavernosum, gonad or penis and be placed distally into the prostatic artery before its branching to the central gland (urethral group of arteries) and peripheral zone (capsular group of arteries). At this point, an additional dose of vasodilator is injected to increase the diameter of the intraprostatic arteries so they can receive more embolic. We have used 5–10mg of isosorbide mononitrate when the microcatheter is at the inferior vesical artery and an additional 5–10mg at the prostatic artery before embolization. Collimation with very slow embolic injection using a 1cc syringe is highly recommended. A negative road map is very useful during embolic injection. Any embolic agent can be used to perform the PErFecTED technique. We have used 300–500μm trisacryl gelatin microspheres. To each 2mL syringe of microspheres, we add 10mL of iodinated contrast medium and 10mL of saline, resulting in a total volume of 22mL with 50% contrast and 50% normal saline solution. We think that a high dilution and very slow injection with a 1cc injection syringe is essential to avoid early proximal occlusion and to obtain diffuse gland parenchymal ischaemia. We do recommend embolizing slowly and reducing fluoroscopy exposure as much as possible. When reaching “near stasis” a manual injection of contrast is performed with a 3cc syringe before proceeding to the second step to observe any collateral shunts.
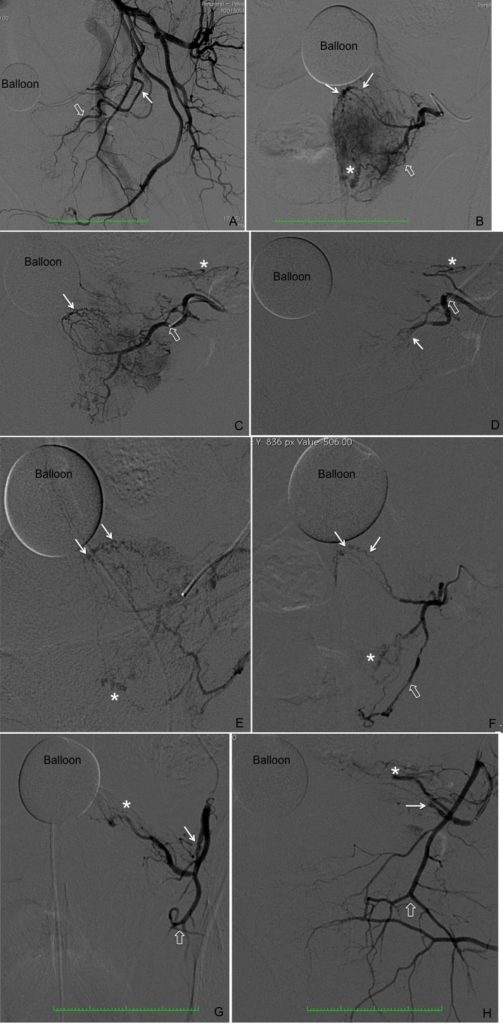
Then, Embolize Distal (Figure 1B)
At this point, the microcatheter should be advanced into the prostatic parenchyma branches for an intraprostatic embolization. Because benign prostatic hyperplasia develops primarily in the periurethral region of the prostate, the urethral group of arteries should be embolized first. The urethral and capsular intraprostatic groups of arteries should be embolized separately. Despite achieving stasis, we have observed that there is potential for prostate enlargement and symptom recurrence after embolization due to microvessels that can recanalise the prostate gland. After moving forward into the intraprostatic branches, a very slow manual injection digital subtraction angiogram may demonstrate some of these microvessels and more embolic can be delivered to block these. Use caution during injection, because shunts opening can be found with the risk of non-target embolization and extravasation may occur if the microcatheter is wedged into the gland. A range from 20–100% additional embolic can be delivered into the prostate gland using this technique. After this second and true stasis, the microcatheter should be retracted to the origin of the inferior vesical artery and a manual contrast injection run performed for final control and to search for additional prostatic branches Figure 2 shows all the angiographic steps when performing the PErFecTED technique.
Francisco Carnevale is associate professor of Medicine, University of São Paulo, São Paulo, Brazil, and director, Interventional Radiology Fellowship Programme. He designed the PErFecTED technique and reports no disclosures pertaining to this article.












