Six-month outcomes from the ongoing CLOUT registry demonstrate the “safety and efficacy” of the ClotTriever thrombectomy system (Inari Medical) in a real-world deep vein thrombosis (DVT) population regardless of clot chronicity level, the 2022 annual meeting of the American Venous Forum (AVF; 23–26, Orlando, USA) heard.
David Dexter (Eastern Virginia Medical School and Sentara Vascular Specialists, Norfolk, USA) was delivering the latest subgroup analysis update from the prospective, multicentre study on behalf of the CLOUT registry investigators based on the first 250 patients enrolled at 24 sites. “We were able to meet the performance goal of greater than 75% in all three [chronicity] groups,” Dexter told attendees. “We had remarkably low device-related serious adverse events at one month. And our rates of post-thrombotic syndrome [PTS]—including moderate to severe—at six months were similarly low.”
The data from the registry show 33% of the 250 patients with acute thrombus, 35% with subacute and 32% with chronic.
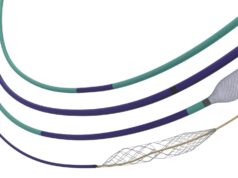
Almost all procedures were single session, with an average of four passes using the ClotTriever device for all chronicity subgroups, Dexter said. No patients required adjunctive thrombolytics. Adjuvant angioplasty was used in 73% (acute: 70%; subacute: 68%; chronic: 84%) and stents in 47% (acute: 46%; subacute: 42%; chronic: 50%) of cases.
Complete or near-complete thrombus removal was achieved in 85% (acute: 90%; subacute 81%; chronic: 84%) of limbs, including 51% (acute: 54%; subacute: 49%; chronic: 49%) with 100% thrombus removal. The post-thrombectomy median hospital stay was one day for all subgroups.
At six months, 90% (acute: 86%; subacute: 89%; chronic: 96%) of the treated limbs had flow present, and 90% (acute: 84%; subacute: 90%; chronic: 91%) were compressible. Any PTS at six months was about 20% in the acute, 25% in the subacute and 30% in the chronic arms. “Statistically, this has a p value of 0.5—we will see how that holds out in another two years when we have finished enrolment of 500 patients,” Dexter said. On the other hand, moderate-to-severe PTS, “was remarkably low at 5% in the acute arm, and about 10% in the subacute and chronic arms.”
Major adverse events and serious adverse “were similar and also rare,” Dexter added. “All-cause mortality was three patients throughout the first 250.”
Furthermore, in terms of venous clinical severity score (VCSS) scores, at 30 days and six months numbers were “nicely low” at 3 and 2 for the acute group, 4 and 3 among subacute patients, and 4 and 4 in the chronic subset, Dexter pointed out. Pain score numbers were “essentially zero across the board.” The same was true when measuring quality of life, he said. “The average quality of life went back to the patient’s baseline regardless of the chronicity believed to be in the clot for acute, subacute and chronic.”
The CLOUT registry’s follow-up out to two years is ongoing. Total enrolment of 500 patients at up to 50 sites has the intention of probing all-comers—across acute, subacute and chronic clot subgroups.