The addition of SIR-Spheres (Sirtex) to chemotherapy has been shown to significantly prolong progression-free survival in the liver among patients with non-resectable liver-dominant or liver-only colorectal cancer in the SIRFLOX study. These results have been published online in the Journal of Clinical Oncology.
Early results of the SIRFLOX study with SIR-Spheres Y-90 resin microspheres were reported during an oral abstract presentation at the 2015 American Society of Clinical Oncology Annual Congress (ASCO; Chicago, USA).
Lead author and the study’s co-principal investigator, Guy A van Hazel, University of Western Australia, Perth, Australia, says, “In the primary endpoint of the study, patients with non-resectable liver-dominant or liver-only colorectal cancer who received FOLFOX-based first-line chemotherapy alone had a median progression-free survival (PFS) at any site of 10.2 vs 10.7 months in those that received chemotherapy plus SIR-Spheres, but this difference was not statistically significant. However, the addition of SIR-Spheres Y-90 resin microspheres to chemotherapy significantly prolonged PFS in the liver, from a median of 12.6 months in the chemotherapy control arm compared to 20.5 months in the SIR-Spheres arm, which translated to a 31% reduction in the risk of tumour progression in the liver. Long-term disease control is critical as liver metastases eventually cause the death of the majority of the hundreds of thousands of patients who get colorectal cancer that cannot be removed by surgery.”
Gilman Wong, chief executive officer of Sirtex Medical, says that, “We remain hopeful that our pre-planned, combined analysis of the SIRFLOX data with the findings of the FOXFIRE and FOXFIRE Global studies, which will be available in 2017, will give us a clear indication of the survival benefit associated with adding SIR-Spheres Y-90 resin microspheres to a standard-of-care chemotherapy.”
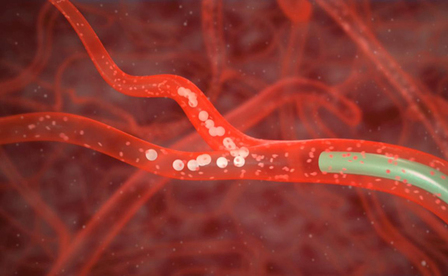
The SIRFLOX study recruited 530 patients who had been diagnosed with unresectable mCRC at 87 medical centres in Australia, Europe, Israel, New Zealand, and USA, between October 2006 and April 2013. Of these 530 patients, 263 control patients were randomised to be treated with the mFOLFOX6 regimen of 5FU, leucovorin and oxaliplatin, with the biological agent bevacizumab allowed at local investigator’s discretion. The other 267 patients received selective internal radiation therapy (SIRT) with SIR-Spheres Y-90 resin microspheres in addition to the mFOLFOX6 chemotherapy regimen (± bevacizumab).
The primary endpoint of SIRFLOX was PFS at any site. Patients in the SIRFLOX control arm had a PFS at any site of 10.2 vs 10.7 months in the SIRT arm, but this difference was not statistically significant, with a hazard ratio (HR) of 0.93 and a p-value of 0.43.
However, in respect to the study’s key secondary endpoint of median PFS in the liver, which is the organ that SIR-Spheres Y-90 resin microspheres directly targets, was 12.6 vs 20.5 months in control vs SIRT by competing risk analysis. The HR was 0.69 (p=0.002), representing a 31% gain with the addition of SIRT. In addition, while objective treatment response rate (ORR) at any site was similar (68.1% vs 76.4% in control vs SIRT; p=0.113), ORR in the liver was improved with the addition of SIRT (68.8% vs 78.7% in control vs. SIRT; p=0.042), with complete responses in the liver increased over three-fold (1.9% vs 6.0% in control versus SIRT; p=0.020).
Grade ≥3 adverse events were reported in 73.4% and 85.4% patients in control vs SIRT (P = 0.516), including recognised SIRT-related effects. The safety profile of the combined therapy was noted by the investigators as being as expected and consistent with previous studies.
Van Hazel and his co-authors conclude that, “The median 20.5 month liver PFS for patients treated with chemotherapy plus SIRT represents a substantial prolongation of local disease control compared to systemic chemotherapy alone, which was a median 12.6 months.”
Van Hazel and his colleagues note that overall survival is a secondary outcome for the SIRFLOX study, and that, “During the seven-year recruitment period of the study, when it became evident that improved patient care and new chemotherapy regimens were extending survival for mCRC patients receiving first-line chemotherapy treatment, a decision was made to pre-plan a combined survival analysis including data from SIRFLOX and two additional randomised studies, FOXFIRE and FOXFIRE Global.”
“In all three studies,” they state, “SIRT has been added to oxaliplatin-based chemotherapy in an almost identical patient population. The FOXFIRE and FOXFIRE Global studies have completed accrual and combined with SIRFLOX have a total recruitment of over 1,100 patients; this provides adequate power to detect a survival advantage,” with findings expected to be reported in 2017.












