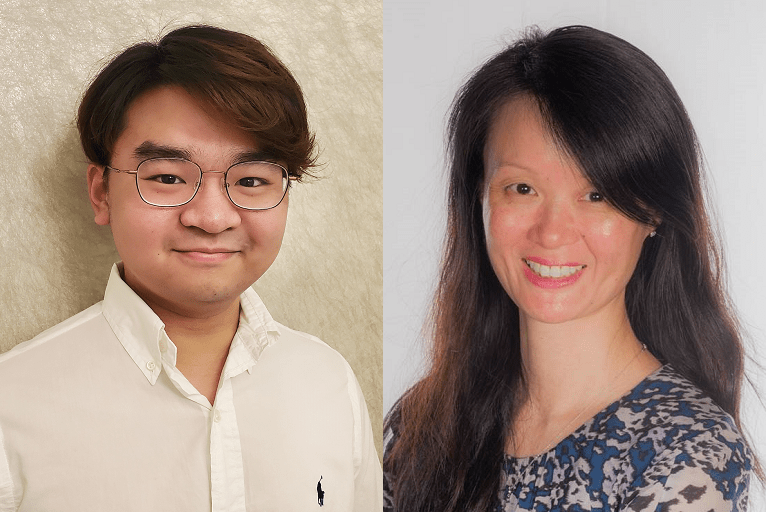
In light of recent and upcoming developments in the space, Vinson Wai-Shun Chan and Tze Min Wah (Leeds, UK) explore the evidence and latest progress in renal tumour biopsy (RTB), and discuss the treatment of small renal masses (SRMs) more broadly.
The optimal diagnostic pathway and treatments for small renal masses (T1N0M0) is controversial. Due to the lack of tumour markers and inability to determine malignancy from benign pathologies, SRMs are often over-treated. Yet, RTB has not been widely implemented into the diagnostic pathway of SRMs. In terms of treatment, partial nephrectomy remains the gold standard for curative surgery but is associated with significantly reduced renal function and high complication rates. Although high-quality evidence is lacking, percutaneous image-guided ablation (IGA) provides excellent oncological, perioperative, and renal function outcomes.
As a result of increased used of abdominal imaging, the rates of incidentally discovered SRMs have increased over the past decade. However, there is no reliable imaging or tumour markers to determine the lesion’s malignant potential. Further, it was shown that over 20% of these treated masses are benign in histology, suggesting significant overtreatment of patients without malignant disease. A systematic review and meta-analysis have reported that diagnostic core biopsies have a sensitivity and specificity of 99.1% and 99.7%, respectively, for malignancy. Despite the proven accuracy and safety profile of RTB, there is reluctance to implement RTB within the urological community.
The benefits of performing RTB before treatment is at least twofold. First, this can guide patient decision-making on whether to receive treatment. More than 90% of interviewed patients with SRMs have expressed that they believe knowing the mass’ histology status will aid decision-making for the optimal treatment. Secondly, given a malignant result for RTB, an RTB can guide the best treatment for the patient, where low-grade SRMs could opt for active surveillance or IGA; and high-grade SRMs could opt for partial or radical nephrectomy. In fact, the latest study of the EuRECA registry1 showed that, amongst patients undergoing ablation, the pre-cryoablation biopsy rate rose from 42% in 2015 to 72% in 2019 (p<0.001). Subsequently, patients are less likely to be overtreated for benign disease when more biopsies are performed (odds ratio [OR]=0.64, p<0.001).
This has shown promising potential in extending the use of preoperative RTB to other forms of SRM treatment—especially partial nephrectomy—avoiding the significant decline in renal function and high complication rates post-nephrectomy. However, it is important to stratify patients who will benefit the most from biopsies. For example, patients over the age of 70 or who are unfit to undergo definitive treatment for SRM may not benefit from RTB; while those with complex tumours or comorbidities may benefit from RTB to prevent complex, high-risk treatments in these patients.1
Since the introduction of image-guided radiofrequency ablation (RFA) in 1998, the technology of IGA has developed significantly to include multiple different energy sources including cryoablation, microwave, and irreversible electroporation (IRE).2 The advantages of IGA compared to partial nephrectomy are at least twofold. Firstly, IGA is significantly less invasive compared to partial nephrectomy, with significantly reduced complication rates.3 Secondly, IGA is associated with a significantly lesser drop in renal function, which is crucial in patients with bilateral (synchronous or asynchronous) disease, or those who require repeat treatments—such as Von-Hippel Lindau syndrome (VHL) patients.
However, there is a lack of high-quality evidence to support the oncological non-inferiority of IGA compared to partial nephrectomy. This could be due to a few reasons. Firstly, previous recruitment of various trials involving IGA has failed, notably in the SURAB and the CONSERVE studies, which could be a result of patient preferences and lack of evidence at the time to support the recruitment process. Secondly, as pointed out by a review performed by the European Association of Urology (EAU) Renal Cancer working group, the quality of observational studies and systematic reviews on the area is poor, notably affected by severe selection bias whereby younger and fitter patients tend to receive partial nephrectomy, compared to old and frail patients receiving IGA. Similarly, the latest systematic review and meta-analysis, published in the International Journal of Surgery, has suggested the same.3
Based on the limited quality of evidence on T1a SRMs, ablation is associated with similar cancer-specific survival, metastasis-free survival and disease-free survival compared to partial nephrectomy. Local recurrence-free survival is similar to partial nephrectomy patients with a follow-up of more than five years.3 Patients undergoing ablation also experience significantly less postoperative complications (risk ratio [RR]=0.72, p=0.02) and significantly smaller decline in renal function postoperatively (mean difference [MD]= -7.42, p<0.01).
Similarly, the long-term outcomes at our centre from 2003 to 2020 have shown similar outcomes, with overall survival, cancer-specific survival, local-recurrence free survival and metastasis-free survival in IGA at least as good as partial nephrectomy, with significantly better renal function preservation.4 Specifically, IGA is of use in patients with Von-Hippel Lindau syndrome—shown in the 17 patients who underwent IGA for VHL-associated renal cell carcinoma (RCC) and experienced excellent oncological outcome without the need for renal dialysis over 10 years of follow-up.5
The role of RTB and IGA has developed significantly throughout the last two decades; however, further research is required to consolidate the role of RTB and IGA in the treatment of SRMs. Firstly, RTB needs to be implemented in both research and clinical pathways. RTB can act as index tests for future diagnostic studies to facilitate development of new imaging modalities. For future interventional studies of new treatments, RTB will also allow focused research on RCC, rather than undifferentiated SRMs alone to improve the quality of evidence. Secondly, studies reporting outcomes from interventional oncology studies must conform to the CONSORT guidelines to allow for meta-analysis and further discussion of the data. Finally, urologists and interventional radiologists should work closely together to embrace and produce optimal outcomes for patients presenting with RCCs. Upcoming results from the NEST trial comparing the effectiveness of nephron-sparing surgeries and future research studies are highly anticipated.
References:
- Chan V W-S, Keeley F X, Lagerveld B et al. The changing trends of image-guided biopsy of small renal masses before intervention—an analysis of European multinational prospective EuRECA registry. Eur Radiol. 2022; 5:1–12.
- Wah T M, Lenton J, Smith J et al. Irreversible electroporation (IRE) in renal cell carcinoma (RCC): a mid-term clinical experience. Eur Radiol. 2021; 31:7491–9.
- Chan V W-S, Abul A, Osman F H et al. Ablative Therapies versus Partial Nephrectomy for Small Renal Masses—a systematic review and meta-analysis of observational studies. Int J Surg. 2022; 97:106194.
- Chan V, Osman F, Cartledge J et al. Percutaneous image guided cryoablation and radio-frequency ablation versus partial nephrectomy for small renal cell carcinomas: A ten-years, single centre observational study. J Urol. 2021; 206(3): 770–1.
- Chan V W-S, Lenton J, Smith J et al. Multimodal image-guided ablation on management of renal cancer in Von-Hippel-Lindau syndrome patients from 2004 to 2021 at a specialist centre: A longitudinal observational study. Eur J Surg Oncol. 2021. Doi: https://doi.org/10.1016/j.ejso.2021.10.022.
Vinson Wai-Shun Chan is a final year medical student in the School of Medicine in the Faculty of Medicine and Health at the University of Leeds in Leeds, UK.
Tze Min Wah is a professor, and senior consultant diagnostic and interventional radiologist, in the Department of Diagnostic and Interventional Radiology in the Institute of Oncology at St James’s University Hospital, Leeds Teaching Hospitals NHS Trust, in Leeds, UK.
The authors declared no relevant disclosures pertaining to this article.










