Findings presented at the Leipzig Interventional Course (LINC; 22–25 January 2019, Leipzig, Germany) contradict the results of a meta-analysis published in the Journal of the American Heart Association in December 2018 linking paclitaxel-coated devices and increased mortality. Several presentations to LINC attendees showed data supporting the use of paclitaxel-coated devices to help the more than 200 million patients globally who have peripheral arterial disease (PAD).
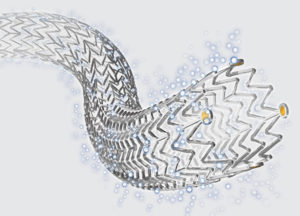
Data were presented on specific paclitaxel-eluting devices. Michael Dake, the principal investigator for the Zilver PTX randomised controlled trial and a paid consultant for Cook Medical, presented results demonstrating the safety and effectiveness of the Zilver PTX drug-eluting stent (Cook Medical). The trial amassed data on 479 patients in a five-year follow-up randomised controlled trial. A separate, recently released Japanese five-year post-market study on Zilver PTX showed positive long-term safety and effectiveness outcomes in challenging real-world patients.
After reviewing all patient level data in the Zilver PTX five-year follow-up, Dake stated that “Cook’s patient level data demonstrate no increased mortality rates at five years with use of a Zilver PTX paclitaxel-coated stent versus the use of non-coated stents and balloons.”
Zilver PTX is indicated for improving luminal diameter for the treatment of de novo or restenotic symptomatic lesions in native vascular disease of the above-the-knee femoropopliteal arteries having reference vessel diameter from 4mm to 7mm and total lesion lengths up to 300 mm per patient.
“We believe industry-wide discussion on topics related to patient safety and long-term patient outcomes are critically important. In the case of paclitaxel, we have studied this drug for more than 20 years and tens of thousands of patients have been treated with Zilver PTX,” comments Mark Breedlove, vice president of Cook Medical’s vascular division. “The recently published meta-analysis linking paclitaxel-coated devices and increased mortality didn’t include patient-level data.”










