The largest study of its kind to date shows that minimally invasive radioembolization may slow metastatic disease progression in liver when no other treatment options remain, according to research being presented at the Society of Interventional Radiology’s 39th Annual Scientific Meeting (22–27 March, San Diego, USA).
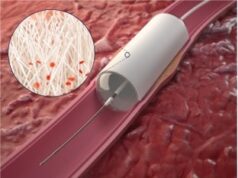
In the largest study of its kind to date, researchers reviewed treatment outcomes of 75 women (ages 26–82) with chemotherapy-resistant breast cancer liver metastases, which were too large or too numerous to treat with other therapies. The outpatient treatment, SIRT that is also called Y90 radioembolization, was safe and provided disease stabilisation in 98.5% of the women’s treated liver tumours.
“Although this is not a cure, Y90 radioembolization can shrink liver tumours, relieve painful symptoms, improve the quality of life and potentially extend survival,” said Robert J Lewandowski, associate professor of Radiology at Northwestern University Feinberg School of Medicine, Chicago, USA. “While patient selection is important, the therapy is not limited by tumour size, shape, location or number, and it can ease the severity of disease in patients who cannot be treated effectively with other approaches,” he said.
While chemotherapy is the standard treatment for patients with metastatic breast cancer, many will either have progressive liver disease despite multiple different treatment regimens while others will not tolerate the side-effects from toxic agents. Currently, patients are considered for Y90 radioembolization when they have no other treatment options, he said.
“The value of Y90 radioembolization in treating patients with non-operative primary liver cancer and metastatic colon cancer has been demonstrated,” said Lewandowski. Given the low toxicity and high disease control rates, this therapy is expanding to other secondary hepatic malignancies, he said. “We are looking to gain maximal tumour control while minimising toxicity and preserving quality of life,” he added.
In this study, imaging follow-up was available for 69 of the 75 women treated. In all of these women, liver tumours were growing prior to treatment. Following radioembolization, there was disease control in 98.5% of the liver tumours, with more than 30% reduction in tumour size for 24 women. The treatment had few side-effects.
“Y90 warrants further study of its efficacy in providing supportive care to relieve patients of debilitating symptoms and control the progression of their disease,” said Lewandowski.