The ability to achieve bleeding control in critically ill patients seems to depend chiefly on early intervention and severity of the underlying disease, such as coagulation disorders. Previous surgery for bleeding is also a well-documented independent predictor of poor embolization outcome, writes Romaric Loffroy, Dijon, France.
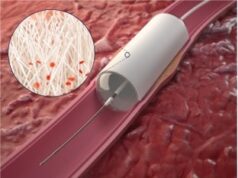
Transcatheter arterial embolization has been performed worldwide for at least three decades and has been shown to be effective at controlling acute arterial upper and lower gastrointestinal bleeding and decreasing mortality. Although few published series have analysed factors predicting embolization failure, there are now enough data on factors that may influence the outcome of patients who have undergone embolization procedures for acute gastrointestinal haemorrhage.
Among clinical predictors of rebleeding, coagulopathy has been shown to adversely affect the success rate for embolotherapy, with an increase in the odds ratio for clinical failure, which ranges from 2.9 to 19.6. Consequently, every effort should be made to correct coagulopathy before, during, and after intervention.
Other clinical variables have been identified as predictors of early rebleeding after embolization. Several of the variables that were studied in our largest series such as coagulation disorders, a longer time from shock onset to angiography, a larger number of units of red blood cells transfused before angiography, and having ≥2 comorbid conditions were found to be associated with early rebleeding. Thus, the ability to achieve bleeding control in critically ill patients seems to depend chiefly on early intervention and severity of the underlying disease. Previous surgery for bleeding is also a well-documented independent predictor of poor embolization outcome.
Clinical signs of shock and active bleeding at admission are known risk factors for rebleeding after endoscopic therapy; hence, they are probably risk factors for early recurrence after embolization as well. Corticosteroid use is more often encountered in inpatients with bleeding than in those with primary-referred gastrointestinal haemorrhage, but it has not yet been reported to be an independent risk factor for rebleeding.
Regarding technical predictors of rebleeding, blind embolization is controversial. Because massive bleeding is often intermittent, most groups have adopted a policy to embolize on the basis of endoscopic findings even in situations where no extravasation is seen angiographically. Based on the findings from the literature and our own experience, we believe that blind embolization is appropriate.
Marking the site of bleed with a metallic clip can assist with localization of the vessel feeding the bleeding ulcer even if there is no contrast medium extravasation. The only limitation of this technique is the need for around-the-clock availability of an experienced gastroenterologist, which is easy to achieve only in high-volume medical centres.
More controversial is the influence of the type of embolic agent on the clinical outcome. Encarnacion et al achieved a low success rate in their series, which included mostly patients embolized with gelfoam alone. These data confirm that the use of gelatin sponge as the only embolic agent guarantees only short-term results and should probably be avoided. The literature supports the use of gelfoam in association with coils when choosing a strategy for the subgroup of patients with bleeding from the gastroduodenal artery. We demonstrated that the use of coils as the only embolic agent was significantly associated with early rebleeding in the upper tract. Coils probably should not be used as the only embolic agent but rather in association with gelfoam for the treatment of gastroduodenal hemorrhage, especially when using the sandwich technique. More recently, the use of n-butyl cyanoacrylate glues as Glubran2 or Trufill has gained acceptance, with very good results in both upper and lower gastrointestinal bleeding. Furthermore, the time for embolization using glue is significantly quicker than for procedures that do not use glue. This is important particularly in cases of massive bleeding that require urgent haemostasis, especially in patients with coagulopathy.
Factors influencing mortality include advanced age, trauma or sepsis, recent major operation, lung or liver disease, and massive blood transfusions. A number of factors have been identified as influencing postembolization mortality. One of the most important and frequently encountered is the absence of early recurrent bleeding. A strong correlation has been seen between coagulopathy, clinical failure, and mortality after embolization.
In conclusion, several factors must be known by interventional radiologists because they may influence the clinical outcome of embolotherapy in such setting. Specifically, every effort should be made to perform embolization early after bleeding onset and to correct coagulations disorders. In addition, careful selection of the embolic agents according to the bleeding vessel may also play a role in a successful outcome.
Romaric Loffroy is a full professor of Radiology, section head of Interventional Radiology, Department of Vascular, Oncologic and Interventional Radiology, Bocage University Hospital, Dijon, France. He has reported no disclosures pertaining to this article.