
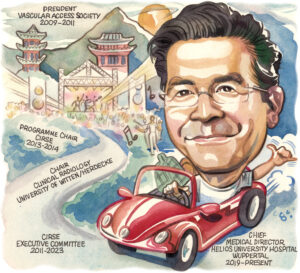
As a champion of innovation and forward movement in his chosen field of interventional radiology (IR), Patrick Haage’s career is no less a reflection of this ideology. With an interest in vascular access, state-of-the-art imaging technologies and artificial intelligence (AI), Haage’s research throughout his career has looked to steer many domains toward progress. Haage is also active in education on a national and international level through leadership roles within multiple scientific conferences and as a founding member of the European Board of Interventional Radiology (EBIR). Set to receive the Distinguished Fellow award at this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (14– 18 September, Lisbon, Portugal), Haage speaks to Interventional News to share key moments from his career so far.
What attracted you to a career in IR?
During my medical studies, I developed an interest in less invasive surgical procedures that enable substantial interventions through small incisions. Simultaneously, I was deeply impressed by the scope of radiology as a field and its potential for interdisciplinary and multidisciplinary collaboration. As a radiologist, one has the unique ability to both diagnose a disease and offer therapeutic interventions. The opportunities presented by this discipline appeared to be the ideal path forward for me at that time, and I am happy to affirm today that it was indeed the correct decision. In my view, interventional radiology (IR) offers an unparalleled blend of innovation, technology, patient care, problem-solving, diversity, and constant advancement.
Who were your mentors?
Throughout the years, professor Rolf W Günther, former chairman of radiology at the Rheinisch-Westfälische Technische Hochschule (RWTH) Aachen University in Aachen, Germany, has been a mentor of mine, having previously been my academic teacher and later friend. Professor Dierk Vorwerk Klinikum Ingolstadt in Ingolstadt, Germany, who is the former head of IR at RWTH Aachen University who also supported me in my clinical and scientific development from day one.
Could you describe a particularly memorable case of yours?
There are many cases that have stayed in my memory. Every single event, whether positive or negative, has contributed to my development. The combination of these experiences has shaped me into the person I am today.
I have been very fortunate to never have permanently harmed a patient due to an avoidable complication over all these years, even in difficult situations that I encountered for the first time. Therefore, every procedure that I was allowed to perform as lead interventional radiologist for the first time was memorable—my first dialysis patient, my first gastrointestinal bleed, my first cava filter, my first thrombectomy, my first transjugular intrahepatic portosystemic shunt.
I also had the great fortune to be the first interventional radiologist in Aachen to insert an aortic prosthesis endovascularly. In collaboration with vascular surgeons at my centre, we spent a long morning in the angiosuite successfully inserting this prosthesis. I am still amazed at how confidently the team and I took on this challenge. This is not only a matter of attitude but perhaps also the privilege of the young.
 Having been involved in several CIRSE committees for many years, how has the programme adapted to scientific innovation and what key developments stick out in your memory of previous congresses?
Having been involved in several CIRSE committees for many years, how has the programme adapted to scientific innovation and what key developments stick out in your memory of previous congresses?
CIRSE has a long tradition of adapting its programmes to scientific innovation by incorporating the latest advancements in IR and related fields into its congresses and events. This includes hot-topic symposia, hands-on workshops, and presentations on emerging technologies, techniques, and research in the field.
Key developments that stick out in my memory from previous CIRSE congresses include the introduction of ever-new minimally-invasive procedures, paired with advancements in imaging technologies, breakthroughs in the treatment of emergency, tumour and paediatric conditions. Particularly exciting has been the implementation of prostatic artery embolization and more recently musculoskeletal embolization and its direct impact on patient well-being.
The integration of artificial intelligence (AI) and machine learning in IR practices will significantly impact the way interventional radiologists diagnose and treat patients. I believe that this technology will ultimately lead to improved outcomes, time and money savings and improved patient care. In the end however, the patient-doctor relationship will remain as an non-negotiable part of the diagnostic, and especially therapeutic, road to restitution.
As one of the founding members of EBIR, how important is the standardisation of education for IR and how do you feel the EBIR examination has influenced IR practice?
Ensuring that practitioners of IR possess the required knowledge and skills to deliver top-notch patient care is essential. EBIR plays a vital role in this process by establishing educational standards, creating curricula, and conducting examinations to evaluate the proficiency of IR specialists. Since 2010, the EBIR exam has had a hugely beneficial impact on IR practice in various ways. Firstly, it guarantees a consistent level of knowledge and expertise among IR specialists, throughout not only Europe, but worldwide, fostering uniformity and excellence in patient care. Secondly, the exam promotes ongoing learning and professional growth among interventional radiologists as we strive to meet the high standards set by the EBIR. Additionally, the EBIR exam offers a respected credential that showcases the proficiency and competency of IR specialists to patients and other healthcare professionals. This has boosted the reputation of IR as a specialised field within radiology and attracts talented individuals to pursue a career in IR.
Overall, the standardisation of education through the EBIR exam has positively influenced IR practice by campaigning for excellence, ensuring know-how, and elevating the overall standard of care provided to patients. The newly established European Certification for Endovascular Specialists (EBIR ES) serves as a validation of an interventional radiologists’ knowledge, experience, and competency in performing complex endovascular procedures, and thus not only enhances our credibility and reputation, but also radically increases our visibility for patients, colleagues, and healthcare institutions.
You are also a co-founder of the European Conference on Embolotherapy (ET) conference which just recently commenced. What were the priorities of this year’s meeting and were there any particularly exciting data releases?
Founded by Christoph Binkert in 2019— with a little help from myself —ET is typically focused on in-depth discussion of the latest research findings, advancements in embolization procedures, updates on imaging technologies for embolotherapy, and the management of complex cases using embolization techniques.
At the 2024 ET meeting in Vienna, some of the data releases and presentations included new research on the efficacy of embolization procedures, advancements in imaging technologies for embolotherapy, and updates on the management of complex cases using embolization techniques. Some of the main foci this year were the treatment of haemorrhoids, lymphatics, endoleaks and musculoskeletal pathologies. The newly added “deep-dive” sessions intensified the teaching and learning aspect for attendees.
Several of your recent research papers have considered the place of AI and machine learning in IR. How do you feel these technologies will interact with IR in the future? Should interventional radiologists have any reservations in embracing this technology?
AI and machine learning have the potential to greatly impact our field by improving efficiency, accuracy, and outcomes. These technologies can help in image interpretation, treatment planning, and decision-making. In the future, AI algorithms and machine learning should play a significant role in IR by automating routine tasks, assisting in complex procedures, and providing personalised treatment options. Interventional radiologists should not have reservations in embracing AI and machine learning technology. Instead, they should see it as a tool that can enhance and improve their existing skills. Nevertheless, it is important for interventional radiologists to receive proper training on how to effectively integrate these technologies into their practice. Plus, they should also be aware of the limitations and potential biases of AI algorithms, and use them as a supplement to their own expertise rather than a replacement.
With decades of experience in IR education, what, in your opinion, is the most underserved/underresearched area of IR?
Generally, I find the development of our community and society in the last 20 years as breathtakingly positive. Interventional radiologists are constantly reinventing themselves by opening up multiple intelligent and less invasive treatment possibilities that are beneficial to the patient. If I should name one area I find underserved and in need of more attention it is paediatric IR.
Paediatric patients have unique anatomical and physiological considerations that require specialised care and tailored interventions. As of now, there is a limited amount of research and few dedicated training programmes focused on paediatric IR compared with adult programmes. In my years as scientific programme committee member and chairman I have tried to push paediatric IR training into attention. This development should be continued.
What piece of advice would you give to early-career interventional radiologists today?
As I’ve mentioned, IR is rapidly evolving. Thus, focus on continuous learning and professional development is key. Actively attend national and international conferences and workshops. Pursue additional training and certifications and advance your skills. Engage in research and academic activities, publish scientific papers and present your work at conferences to contribute to the advancement of IR. This will give you the benefit of expanding your network. Seek mentorship and guidance as you navigate your early career. Finally, always welcome innovation and technology, stay ever curious so that you can deliver cutting-edge care to your patients. Don’t let yourself be changed, be part of the change.
What are your interests and hobbies outside of your career?
Outside of my work I enjoy spending time with my family (my two sons Noah and Jona, and wife Nadja) or my friends. I like to travel, particularly to Asia and Korea. I also enjoy sports such as skiing or tennis, and driving fast cars—or old ones, (Porsche 911, Volkswagen Beetle)—and going to big events, such as rock concerts and soccer games.










