In a study evaluating the efficacy of a drug-coated balloon (DCB) in inhibiting restenosis and ensuring long-term patency in patients with arteriovenous fistulae (AVF), the paclitaxel DCB did not show superiority to a placebo high pressure balloon at 12 months’ follow-up. Manuela Moreno-Ramírez (Department of Nephrology, Juan Ramón Jiménez Hospital, Huelva, Spain) presented these results of the EffPAC trial at the Cardiovascular and Interventional Radiological Society of Europe annual meeting (CIRSE; 22–25 September, Lisbon, Portugal).
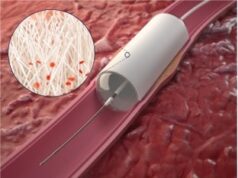
The trial was an investigatorinitiated, prospective, multicentre, double blind, randomised study conducted across four Spanish hospitals. One hundred and seventy-eight dialysis patients included in the study were divided into two groups: those treated with a paclitaxel DCB—the CE-marked Passeo-Lux 18 (Biotronik)—and those treated with an uncoated high pressure balloon, who were recipients of a placebo. The placebo involved the use of a safe and biocompatible non-hydrophilic excipient called butyryl-tri-hexyl (BTHC) that facilitates the delivery and absorption of the drug from the vessel wall.
Moreno-Ramírez emphasised the need for new procedures to treat stenosis, telling the CIRSE audience that “Difficulties with vascular access are an important source of morbidity and mortality in haemodialysis patients. Stenosis could be treated with percutaneous transluminal angioplasty (PTA), but the primary patency rate is only 40–50% at one year—hence, new procedures are needed.” Thus, the study investigators were interested in researching the paclitaxel DCB as a possible alternative treatment strategy.
However, neither the primary nor the secondary endpoints of this study were met, with the paclitaxel DCB failing to demonstrate superiority over the placebo. In addition to the primary endpoints of safety and efficacy, Moreno-Ramírez and colleagues sought to determine differences in survival rates. They found none. Despite the mean survival in the DCB group being higher, at 265 days versus 237, this was not statistically significant. There were therefore no statistically significant differences in survival at 12 months’ follow-up in terms of stenosis location, type of arteriovenous fistulae, or previous angioplasty. Moreno-Ramírez summarised: “We think this result is not clinically relevant.”
This finding is the same as that of another multicentre clinical trial with a significant sample size, conducted by Scott Trerotola and colleagues (Department of Radiology, Perelman School of Medicine of the University of Pennsylvania, Philadelphia, USA). Trerotola concluded in 2018 that, despite finding a slight improvement in survival using the Lutonix DCB (BD) compared to a placebo at six months’ follow-up, the difference was not statistically significant. However, several other previous studies, such as the IN.PACT trial by Panagiotis Kitrou (University of Patras, Patras, Greece) and colleagues—investigating at the In.Pact Admiral DCB (Medtronic) versus a placebo—contradict this conclusion, finding a definite improvement in survival with a DCB compared to uncoated alternatives.
However, Moreno-Ramírez does believe it is important to note that the global survival rates in her team’s study at 12 months are superior to that in previous published studies, at almost 60%. Moreno-Ramírez attributed this to the use of a high pressure balloon for angioplasty. Clarifying her methodology, Moreno-Ramírez explained that for every patient enrolled in the present study, both those in the DCB arm and the placebo arm, the first angioplasty utilised a high pressure balloon. Next, Moreno-Ramírez and colleagues carried out a fistulography to discover if the first angioplasty had been effective. Allocation into the two different randomised groups occurred then, before a second angioplasty with DCB.