By Steven Rose
In order to meet a need for transcatheter embolic agents that can be precisely placed, optimally conformed, with complete and durable occlusion, and maximal safety profile, several notable developments have occurred with respect to coil-type embolization. A generic overview of commercially available devices follows.
With respect to safety and precision of coil placement, the most important advancement has been the feature of the elective controlled coil detachment. Specifically, the coil remains attached to the pusher wire component until deployment is both complete and satisfactory, at which time the coil is released. Release mechanisms vary, and may be passive interlocking components that fall apart when advanced beyond the catheter tip, or elective detachment using mechanical or electrical means. Should a coil deploy unsatisfactorily, this feature allows the operator to retract the coil, then either re-attempt deployment or remove the coil all together. The controlled detachment feature allows one to attempt coil placement in higher risk situations such as a limited “landing zone” or with suboptimal catheter purchase into the targeted blood vessel.
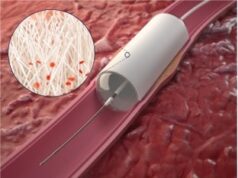
Embolic vascular plugs are an extension of the concept of detachable coils. Specifically they are a tightly woven self-expanding metal (currently nitinol) mesh formed into various plug shapes, with a range of diameters. The currently available plugs are attached to the pusher wire with a screw mechanism that is unwound at the time the operator wishes to release the device. In general, these plugs are designed for use in larger diameter, higher flow vessels such as lobar portal vein branches or large gastroesophageal varices.
Most currently available coils are either bare metal or incorporate various synthetic fibres to promote thrombosis. Nevertheless, failure to cause complete occlusion or delayed recanalisation can limit their effectiveness. One vendor has incorporated a desiccated layer of hydrogel onto the surface of the coil. When the coil is introduced into a solution with a pH greater than 7.0 (blood has a pH of 7.4), the hydrogen ions leach out and are replaced with water molecules that cause expansion of the hydrogel by factor of approximately four. This feature appears to more predictably cause complete vessel or aneurysm occlusion, reduces delayed recanalisation, and forms a lattice for ingrowth of vascular endothelium.
A significant hurdle to widespread and more generalised use of these advanced coils and plugs is the issue of cost. Pushable fibred platinum coils cost in the range of US$80–$100 each. Detachable fibrous coils sell for approximately US$500–$600 each, and hydrogel coated detachable coils retail in the range of US$800–$900 per coil. Devices intended for neurovascular applications are more expensive yet, typically costing US$1200–$1500 per coil. In this writer’s opinion, situations that warrant use of the high performance, expensive devices are high-risk or anatomically challenging situations that require maximum coil performance in terms of precise, complete vascular occlusion. The cost analysis needs to incorporate the clinical costs of failure to achieve vascular blockage and coil maldeployment.
Alternatively, there appear to be disruptive technologies that may reduce the need for use of expensive, permanent advanced coils.
One such application is the use of temporary anti-reflux tips or occlusion balloon catheters to minimise non-target delivery of Yttrium-90 microspheres into hepatofugal hepatosplanchnic (hepatoenteric) arteries. These devices prevent retrograde reflux of agent into more proximal upstream arterial branches. Additionally, the temporary restriction of antegrade blood flow causes a reduction in the downstream hepatic arterial blood pressure, effecting temporary reversal of blood flow (hepatopedal) in these often difficult to embolize hepatosplanchnic arteries.
In summary, the field of coil embolization is highly dynamic, with currently available elective detachability, vascular plugs for larger vessels, and incorporation of biopolymers. The research has been underway for development of features such as biodegradability and use of coils as a drug delivery platform. Some of the traditional applications of coil embolization may be replaced with blood flow altering devices that provide temporary vascular protection.
Steven C Rose, section chief of the Interventional Oncology Section at University of California, San Diego, USA, will speak on the subject at GEST 2012 US.