By Ian Gillespie
Postpartum haemorrhage is a major cause of maternal death and morbidity. The Confidential Enquiry into Maternal and Child Health (CEMACH) report for 2003–2005 identified 132 maternal deaths in the UK of which 17 were caused by postpartum haemorrhage. In addition to these deaths, serious morbidity may result from massive transfusions, coagulopathy and emergency surgical intervention especially peripartum hysterectomy, and place demands on intensive care facilities.
Postpartum haemorrhage
Most cases which involve interventional radiology occur within 24 hours of delivery (primary postpartum haemorrhage) but haemorrhage may occur up to six weeks post delivery (secondary postpartum haemorrhage) and in this period is usually due to retained products of conception or endometritis. In clinical practice any mother who continues to bleed vaginally or internally (with evidence of expanding pelvic or abdominal haematoma) or becomes haemodynamically unstable should be assessed immediately to identify the site of bleeding and determine the best strategy for haemorrhage control. Early involvement of interventional radiology should be initiated before proceeding to more radical surgical intervention whenever possible.
The main causes of postpartum haemorrhage are:
- Uterine atony after vaginal or caesarean delivery is the commonest cause
- Uterine, cervical, vaginal lacerations
- Retained products of conception
- Post peripartum hysterectomy
- Coagulopathy
Resuscitation and initiation of the local major haemorrhage protocol is the first priority to maintain circulating blood volume and prevent coagulopathy whilst the cause is being assessed. Atony is diagnosed clinically and managed initially by uterine massage and uterotonic drugs. Intrauterine balloon tamponade is often effective but embolization should be considered as an alternative to more radical surgery (uterine B-Lynch brace suturing, surgical ligation of uterine or internal iliac arteries or hysterectomy). Embolization should also be considered early in the management of bleeding from genital tract trauma and post-hysterectomy.
Technical considerations
In atony, focal extravasation of contrast may not be visible but embolization of both uterine or anterior division of both internal iliac arteries is justified. For causes other than atony this author prefers to perform CTA en-route to the angiography suite as this will demonstrate the site of extravasation, vascular abnormalities such as pseudoaneurysm (which may be difficult to identify by subtraction angiography particularly in the presence of arterial spasm), and provide a route map to the site of bleeding. Sources other than internal iliac branches may be identified and procedure time shortened.
Selective embolisation is performed from a femoral route (contralateral is easiest) and gelatin sponge is the agent of choice. Polyvinyl alcohol particles may also be used but avoid less than 300 micron sized particles or liquid agents to minimise the risk of ischaemic complications. Coils are used less often in this clinical scenario and when positioned proximally may allow continued bleeding by distal collateral branches. Flush angiography should be performed prior to completion to ensure there is no bleeding from other arteries, especially if CTA has not been performed.
A recent meta-analysis of conservative treatment options for postpartum haemorrhage found a success rate of 90% for embolization and no significant difference compared to conservative surgical options.
Abnormal placental implantation
This condition results from a defect in the decidua basalis allowing invasion of placental villi into the myometrium. Placenta accreta (adherent to myometrium) accounts for 75% of cases but placenta percreta (invasion through serosa and sometimes into adjacent structures) which occurs in 5% is the most feared and may result in torrential bleeding. The incidence of this condition is increasing due to the rising rate of caesarean section and increasing maternal age. Whilst it may be diagnosed by colour Doppler ultrasound and MRI, its presence may be predicted by the presence of placenta praevia (it is rare in the absence of praevia) and a history of previous caesarean section. Previous sections confer a risk of 40% in one reported series. In the UK Obstetric Surveillance Survey placenta accreta accounted for 38% of peripartum hysterectomies which may result in damage to adjacent bladder, ureters, bowel, and blood vessels.
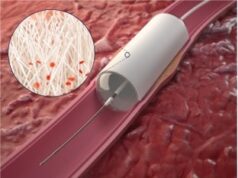
Traditionally, this condition has been treated by caesarean hysterectomy. However, other options include pre-caesarian insertion of balloon occlusion catheters into the anterior divisions of both internal iliac arteries. The balloons may be inflated immediately after delivery and embolisation may be performed through these if necessary allowing the possibility of conserving the uterus or reducing haemorrhage to improve the surgical field for safer hysterectomy. The placenta may be left in-situ in the absence of major bleeding and will involute over time although there is a risk of delayed haemorrhage and infection. Currently there is no clear evidence to support deployment of occlusion balloons and there are anecdotal reports of complications (hypoxic baby, iliac artery occlusion, distal leg emboli, and internal iliac artery rupture). Pending results of further research local protocols which include a role for interventional radiology should be in place to enable delivery under the most controlled conditions.
Conclusion
Pelvic embolisation for postpartum haemorrhage is a safe and effective alternative to radical surgery and interventional radiologists must rise to the challenge of how to provide a robust and readily available service to avoid needless morbidity and the tragedy of maternal deaths.
Ian Gillespie is a consultant interventional radiologist, Edinburgh Royal Infirmary, Edinburgh, UK
Source:‰ÛöEmbolisation UK, 28–30 March 2011, Birmingham, UK