The efficacy and safety of a novel catheter delivering liquid paclitaxel for the prevention of restenosis in below-the-knee lesions has been confirmed by study investigators across 17 sites in the USA. This is the conclusion of the COPPER BTK trial (Occlusion Perfusion Catheter for Optimal Delivery of Paclitaxel for the Prevention of Endovascular Restenosis—below-the-knee), presented by Pradeep Nair of the Cardiovascular Institute of the South Houma (Los Angeles, USA) at the 31st International Symposium on Endovascular Therapy (ISET; 27–30 January 2019, Hollywood, USA).
The occlusion perfusion catheter (Advanced Catheter Therapies) is a universal drug-delivery device. According to an Editor’s note in Vascular Disease Management written by Nair in his capacity as New Technologies Section Editor for the publication, this catheter “allows for delivery of antiproliferative drug[s] to a targeted treatment area, demonstrates exceptional medial layer drug uptake, and can be re-used for multiple treatment sites. Additionally, the outer occlusion balloons prevent downstream washout of antiproliferative agent[s]. Ongoing trials will help establish its role in peripheral arterial disease intervention for both above- and below-the-knee applications.”
The prospective, non-randomised, open-label, multicentre study presented by Nair at ISET aimed to evaluate the efficacy of the occlusion perfusion catheter after atherectomy and percutaneous transluminal angioplasty (PTA) in treating de novo and restenotic below-the-knee lesions, as determined by primary patency at six months. The safety profile of the device was also assessed, defined as freedom from major adverse events at one month. Major adverse events included target lesion revascularisation, major amputation, and target limb related death. A total of 35 patients enrolled in the study, with a mean lesion length of 119.1±80.4mm, and a diameter stenosis of 93.7±8.81%. All patients were in Rutherford class 2–5.
At six months, primary patency was 88%, and the study investigators reported 96% freedom from clinically-driven target lesion revascularisation. There was no target lesion revascularisation, target limb related death, or major amputation in the target limb. The Rutherford classification also improved on average over the course of the study: at baseline, the average Rutherford score was 3.6±0.8, and at six months, the average Rutherford score was 1.8±1.2.
These positive data drew Nair to summarise: “The delivery of liquid paclitaxel using the occlusion perfusion catheter under controlled pressure was technically achievable without procedural complications. The feasibility and initial efficacy of this device provide encouragement for this new technique, with the potential as an alternative approach for infrapopliteal revascularisation. In particular, the ability to treat very long or multi-vessel lesions with a single device could provide a more economical option.”
In addition, he added: “The safety profile in this small cohort study is particularly favourable, and focuses treatment at the target lesion with minimal drug loss that can occur with drug-coated balloons (DCBs).”
Nair acknowledges that longer term follow-up and larger clinical studies will be needed to support the initial findings of this technology with head-to-head comparisons with DCB and balloon angioplasty (with and without atherectomy).
As is common knowledge amongst the interventional community, the optimal strategy for below-the-knee arterial disease remains uncertain. Treatment is impeded by the high incidence of long chronic total occlusions and calcified lesions, meaning previous interventionalists have experienced high restenosis rates and poor-long term clinical patency when treating these difficult lesions. PTA is most commonly employed as a treatment regimen, but, Nair explained at ISET, “often yields non-durable results”. He cited a primary patency of 63% at one-year, less than three-quarters of the six-month primary patency rate observed in the present study with the occlusion perfusion catheter.
Nair noted that DCBs in below-the-knee arteries have historically yielded mixed results, but that several randomised clinical trials in the below-the-knee space evaluating DCBs and scaffolds are ongoing. The main difference between DCBs and the occlusion perfusion catheter used in the COPPER BTK trial is that, while DCBs store antiproliferative agents in the intima, the catheter delivers these therapeutic agents directly to the medial wall.
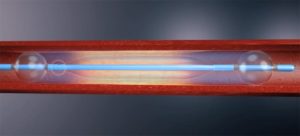
Occlusion perfusion catheter design
The occlusion perfusion catheter is a multi-lumen catheter designed to temporarily occlude the target lesion from blood flow, flush the blood from the treatment chamber, and then locally deliver the therapeutic agents into the artery. It has two compliant occlusion balloons (one proximal and one distal), which define the treatment chamber. The catheter also has one centre space-occupying balloon, which does not contact the vessel wall. Treatment chamber pressure is measured in real-time during infusion of the therapeutic agent via a sensor located within the chamber connected to an external pressure monitor.
Therapeutic agents are infused through the treatment inflow under continuous pressure injection; treatment time is two minutes. The average paclitaxel dose per placement is 6.15mg. Radiopaque markers are located on both side of the occlusion balloons to define the treatment chamber and assist in catheter placement under fluoroscopy.
The occlusion perfusion catheter has FDA 510(k) clearance, and is a 0.014” guidewire compatible, 5Fr device, with an outer diameter of 1.67mm. The device has existed since the establishment of Advanced Catheter Therapies in 2008.
The COPPER BTK study was sponsored by Horizons International Peripheral Group.










