This advertorial is sponsored by Inari Medical.

Evaluating the current standard of care for the management of acute pulmonary embolism (PE) and deep vein thrombosis (DVT), Michael Kostrzewa (Cantonal Hospital Baden, Baden, Switzerland) and Rashid Akhtar (Barts Health NHS Trust, London, UK) discuss the efficacy of mechanical thrombectomy and its expanding application.
Until today, mortality rates for PE remain unacceptably high, sitting between 6–15% for intermediate-high risk and 25–50% in high-risk patients. A similar trend can be observed in patients with DVT, where residual thrombus after treatment can cause long-term issues, with approximately 50% of patients developing post-thrombotic syndrome (PTS) as a result. Standard treatment for PE has typically involved thrombolysis, and for DVT, anticoagulation. However, via technological advances, a better understanding of the importance of new predictors in choosing the right treatment option, and the availability of new tools have begun to shift the focus towards interventional management.
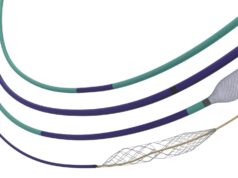
“There are several reasons why we are increasingly intervening on PE and DVT. We have previously never been able to fully extract the clot and characterise its type, l et alone describe the efficacy of tissue plasminogen activator (tPA) on collagen-rich thrombus. Would that clot have been completely dissolved?” Akhtar said. “With the updated toolkits that are now available, such as the FlowTriever® or ClotTriever® systems (Inari Medical) for venous thrombectomy in PE and DVT respectively, it makes treatment more approachable,” Kostrzewa added. In his opinion, these technologies, paired with the positive clinical data and growing evidence, provide treating physicians with the necessary confidence of a reliable and predictable outcome.


At present, data from the FLASH and FLAME registries—which collected data on the use of mechanical thrombectomy with the FlowTriever system for the treatment of acute PE—have shown low rates of all-cause mortality at 30-day follow-up and significantly lower rates of in-hospital adverse events. Similarly in the treatment of DVT with the ClotTriever system, the CLOUT registry shows safety and effectiveness of wall-to-wall thrombus removal, with 93% of patients having no or mild symptoms of post-thrombotic syndrome (PTS) symptoms at two years.
“There’s still a lot to be done,” Kostrzewa said, “but we have good evidence at present and there is very exciting data to come, with the DEFIANCE trial for DVT and the PEERLESS II trial for intermediate-high risk PE patients, as it is often difficult to decide between conservative or interventional treatment. These results will hopefully bring clarity and change the guidelines.”
Touching on the current guidelines and changing the status quo, Kostrzewa believes that awareness is a prevailing issue, which, in his experience, has prevented him and his colleagues from using new and more effective treatment strategies, and has led to a reduced influence on guidelines. “We need to build awareness to change guidelines,” he said, “but I do believe that awareness is changing in the venous thromboembolism [VTE] space, both among the treaters and the non-interventional stakeholders [NISH]. It is all about building an effective and efficient team.”
In Akhtar’s experience, the frequency of mechanical thrombectomy procedures he performs is increasing. “We are in a unique era with the right devices and evolving guidelines, and we are no longer ignoring the mortality figures for PE patients or the prolonged complications that DVT patients face.” Importantly, updates to the European Society of Cardiology (ESC) Guidelines for the diagnosis and management of acute pulmonary embolism from 2019 on mechanical thrombectomy were “a step in the right direction” for Akhtar, helping his team to better assess patients and decide on an informed treatment pathway.
In his institution, he explains, admitted patients are typically administered low molecular weight heparin. Treatment is escalated towards intervention, if the patient shows signs of deterioration within 24–48 hours. They consider factors such as the ratio between right and left ventricle (RV/LV ratio), lactate levels, clot burden and concomitant DVT—all these parameters are essential in their interdisciplinary case discussions and the decision-making process, also known as PE response team (PERT) meetings.
“In the treatment of PE and DVT treatment, interventional radiologists can take the clinical lead, because we see many of these patients and are experts in this field,” Akhtar said. “In my practice, I review patients pre- and post-intervention. You’re getting a DVT procedure with ClotTriever device done within the hour, which is swift and not tedious.” By integrating devices such as the FlowTriever into clinical practice, interventionalists can improve procedural efficiency, Akhtar explained: “It’s useful for interventionalists to do both DVT and PE treatments—I often use the FlowTriever device in DVT interventions. I encourage offering both PE and DVT treatment, as the procedures are straightforward for experienced interventional radiologists. Plus, it’s rewarding. I find that both PE and DVT interventions have renewed my job satisfaction,” he shared.
Kostrzewa points out that the lack of clear guidelines in DVT is a major challenge for referring physicians, as it is not always easy to differentiate between patients who will benefit from interventional treatment and those for whom it is not indicated. “As clinicians, we now have a better understanding of both conditions and what can happen with these patients in the long term. We also have better tools for PE and DVT to safely and efficiently remove thrombus in the lungs and lower extremities,” he states. “Still, we rely on referring physicians to ensure that all VTE patients who are eligible for mechanical thrombectomy, receive this treatment.”.
In Akhtar’s view, a multidisciplinary approach is key to provide PE and DVT patients with optimal care, as interventional techniques such as mechanical thrombectomy shift to become commonplace. Akhtar and Kostrzewa agree mechanical thrombectomy is a game changer in the minimally invasive treatment of PE and DVT, rapidly restoring blood flow and reducing associated risks. Advances in technology, along with further studies, is expected to establish mechanical thrombectomy as a key tool in the management of venous thromboembolic disease, which is expected to be reflected in the future guidelines for the treatment of PE and DVT.
At this year’s Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual congress (14–18 September, Lisbon, Portugal) Inari Medical will be hosting a hands-on workshop on Saturday 14 September, demonstrating the FlowTriever and ClotTriever systems. In addition— on Sunday 15 September—an expert panel will be exploring the impact of mechanical thrombectomy in the management of venous thromboembolism at the 1pm Symposium in Auditorium 2.