In the past, several devices, not designed for thrombectomy, were used as a last resort in stroke treatment. Now, there are devices which have been created specifically for the treatment of embolic stroke, and operator experience with these is growing, Martin Radvany, Division of Interventional Neuroradiology, Johns Hopkins Hospital Baltimore, USA, tells Interventional News.
You have stated that mechanical thrombectomy is no longer a rescue treatment in stroke…could you explain?
Despite the approval of intra venous recombinant tissue plasminogen activator (IV rtPA) for the treatment of stroke, less than 5% of patients receive this therapy in the setting of acute ischaemic stroke. In many cases, it is because the patients do not arrive to the hospital within the three-hour time window for IV rtPA. The ECASS III results have extended this time window to 4.5 hours, but many patients still do not make it to the hospital in time. Intra-arterial tissue plasminogen activator was the next line of treatment and if that failed, various devices, not designed for thrombectomy, were then tried, but only as a last resort, but when all else had failed.
There are now devices which have been created specifically for the treatment of embolic stroke. As operators have become more experienced these devices are being employed immediately when the patient comes to angiography.
What is the background to the problem?
The biggest problem is patient education. Time is critical in caring for stroke patients. As opposed to a heart attack, the symptoms of stroke can be mild. A heart attack is painful and/or uncomfortable and this is what prompts patients to seek medical attention. With a stroke, the symptoms can be much milder, with some minimal extremity weakness that the patient often disregards. It is only when this progresses to the inability to walk or move an arm that patients get concerned enough to seek medical attention.
What are the mechanical thrombectomy devices currently out there and how do they work?
There are many devices in development. In the Unites States there are currently two FDA approved devices. The Merci retriever was the first device approved. It consists of a wire in a spring configuration that is deployed distal to the thrombus and then used to mechanically pull the thrombus from the vessel. The other FDA approved device is the Penumbra system. This device consists of a catheter and a separator, a wire with a cone on the end, which is used to break up the thrombus and then aspirate the pieces through the reperfusion catheter that is attached to a vacuum pump.
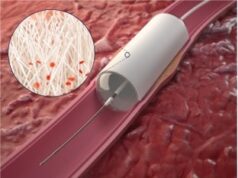
The EKOS catheter has been used in an off-label manner in the United States to treat stroke in the Interventional management of stroke (IMS) studies. The catheter is positioned within the thrombus and then a thrombolytic agent such as rtPA is infused and ultrasound energy is administered via a wire in the catheter expediting clot dissolution.
The last device I will mention is the Solitare Device. It is a self-expanding stent that is currently in trials in the United States and being used elsewhere for the treatment of embolic stroke. The stent is attached to a deployment wire. It can be deployed in an occluded vessel and then used to drag the thrombus from the vessel.
What have the improvements in imaging contributed?
Imaging is playing a larger role in helping to select patients who might benefit from stroke treatment. Initially, CT was used to evaluate patients with stroke symptoms to exclude intracerebral haemorrhage and look for signs of ischaemic stroke which would preclude IV administration of rtPA. As advances have been made in MR and CT imaging, we are now attempting to select patients for treatment based on tissue physiology. The basic idea is that there is a vascular territory that is not being perfused due to vessel occlusion. When stroke imaging is performed, we are attempting to determine the location of the occlusion and delineate the already infarcted tissue from that tissue that will go on to infarction, if we do not restore blood flow. If there is a significant volume of brain tissue at risk of stroke with only a small area of infarction, we would consider intervention past the 4.5 hour window for IV rtPA. Conversely, a patient may arrive within three hours of stroke onset and the physiologic imaging may indicate that the brain tissue in the vascular territory has already undergone infarction and intervention of any kind would not be helpful, and possibly lethal.
What is the current state of evidence regarding mechanical thrombectomy?
Unfortunately, the current evidence regarding mechanical thrombectomy is lacking. The trials that led to the approval of various devices have had small numbers of patients. There are several trials that are underway, or in planning stages, but at this time we need better data.
How would you describe the mechanical thrombectomy and its potential impact on stroke care to colleagues?
Mechanical thrombectomy has the possibility to significantly reduce the morbidity and mortality secondary to stroke. It has already extended the treatment window for stroke patients, and it has the potential to decrease the time it takes to restore blood flow to the brain. One would anticipate that this would lead to improved patient outcomes, but only data from prospective studies will answer this question.