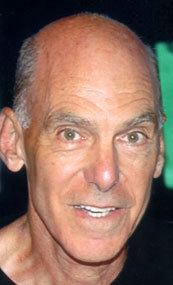
Louis Martin, professor of the Division of Interventional Radiology and Image-guided Medicine, Emory University Hospitals, Georgia, USA, has been awarded with one of the SIR’s Gold Medals 2012. He spoke to Interventional News on his career achievements, memorable cases in interventional radiology and his most interesting research findings.
How did you come to choose medicine as a career? What drew you to interventional radiology?
My father wanted to be a doctor but he graduated from high school during the Depression and could not go to college. He never pressured me to go into medicine, but I knew it would make him very happy if I did, so every time I had an academic choice to make I just kept gravitating in that direction.
Which innovations in interventional radiology have shaped your career?
In 1970 when I completed my diagnostic radiology training there was no such thing as interventional radiology. I took a two year fellowship in neuroradiology which was procedure oriented‰Û¥i.e. angiography, pneumoencephalography, myelography‰Û¥so we were always called upon to perform any new procedure anywhere in the body. The innovations came at very elementary levels: new guidewires, new catheter shapes, better injectors and film changers. The obvious innovations that shaped my interventional career were the angioplasty balloon, the Palmaz stent and later the self-expanding stents, stone baskets and various drainage catheters and procedure sets passed directly from their innovators to us, usually by Cook Medical.
Who were your mentors in interventional radiology and what do you still remember from their wisdom?
My earliest mentors were those who described their innovations to me in an article or a conference presentation such as Charles Dotter, Josef Rösch, Stan Cope and Joachim Burhenne. Later I had the opportunity to practice at Emory University with giants in our field such as Dean Warren, the chairman of the Surgery Department and creator of the Distal Spleno-renal Shunt who gave me a sound background in the treatment of portal hypertension; Andreas Gruentzig the ‘inventor’ of peripheral and coronary balloon angioplasty; Vincent Po Chuang, the best angiographer that I have ever come into contact with; and Bill Casarella our chairman who gave us the opportunity, inspiration, direction and a long enough leash allowing us to reach our potential.
Could you describe an early moment in your career in interventional radiology when you were amazed by what the specialty could achieve?
It has really been a career filled with amazing moments: removing a saddle embolism from the pulmonary arteries of a tachypneic, hypotensive patient; embolizing the source of gastrointestinal haemorrhage; stenting an aortic dissection; treating a patient in sepsis by draining an infected gall bladder, bile ducts or renal collecting system; allowing a child to use their arm or walk without pain by successfully treating a vascular malformation; and many more.
Can you describe a memorable case and how IR came to the rescue?
We were involved over many years treating the visceral aneurysms of a female with intimal medial mucoid degeneration, a rare disease affecting the intima and media of the aortic and extra aortic vessel walls, predominantly occurring in younger African females with hypertension. At last presentation, the right renal artery had avulsed and the aorta directly communicated with a large (18 cm) retroperitoneal pseudoaneurysm. The aortic defect was successfully treated by trapping the neck of the pseudoaneurysm between the discs of an Amplatzer Septal Occluder device.
What are the three most important things you focus on as a teacher of interventional radiology?
- It is an honor and privilege to be allowed to treat a patient. It is our duty to make sure that the treatment is appropriate and performed to the very best of our ability. The patient and their family must be treated with the care and consideration that you would wish for yourself or a loved family member. It is important that they meet the operator before the procedure and are personally informed of the results after it.
- Be honest with the patient and yourself.
- Do not be afraid to ask questions. Search for alternate answers. Be skeptical of those who know the ‘right’ answer, there is frequently more than one.
What have been the three most interesting findings from your research so far, which you would like to share with other interventional radiologists?
- It is possible to distinguish calcium from atheroma and non-atheromatous tissue using Raman spectroscopy. This may be of use in designing the ‘smart’ laser for use in reanalysing occluded arteries and identifying vulnerable plaque.
- Our focus should be in designing the self-adjustable portosystemic shunt that can maintain portal perfusion of hepatocytes at a level ‰ÓÛ high enough ‰ÓÛ to prevent hepatic encephalopathy and ascetic accumulation while maintaining a pressure low enough to avoid variceal haemorrhage.
- Most of our therapies are doomed to eventually fail. They must be administered in an order that maximises their benefit; i.e. it is not always in the patient’s best interest to use the “big gun” during the first encounter.
What are the three most interesting papers you read in 2011 in the field of vascular interventions?
- Wang J, Zhu YQ, Li MH, et al. Batroxobin plus aspirin reduces restenosis after angioplasty for arterial occlusive disease in diabetic patients lower-limb ischemia. JVIR 2011; 22 (7): 987-994
- Tam A, Singh P, Ensor JE, et al. Air travel after biopsy-related pneumothorax: Is it safe to fly? JVIR 2011; 22 (5): 595-602
- Denecke, T, Seehofer D, Grieser C, et al. Arterial versus portal venous embolization for induction of hepatic hypertrophy before extended right hemihepatectomy in hilar cholangiocarcinomas: A prospective randomized study. Top of FormJVIR 2011; 22 (9): 1254-1262
What are your current areas of research?
- Radiofrequency renal sympathetic denervation for refractory essential hypertension. I am a co-investigator at Emory University for the Symplicity 3 trial.
- Treatment of portal hypertension
- Brachytherapy to reduce myointimal hyperplasia.
What are your views on how complications are currently measured in IR, and what improvements do you wish to see in this regard?
I think we do very poorly in evaluating our complications to interventional procedures. Unless we are working under a very strict research protocol, the tendency is to explain away or divert the blame for procedural complications. This is human nature and it is true that the causes of the complications are frequently multifactorial. I think that a major problem is using the word “complication”. It is confrontational and pejorative and immediately places the operator in a defensive position. I think it is much better to use the term “adverse event” which does not inherently assess blame or quantify the event. For example: it is not unusual to incite a transient arrhythmia while placing a central venous line. Is it a complication? Do we really know? The arrhythmia rarely requires medication or electrical conversion and is usually not recorded in the post-procedural dictation. It is therefore impossible to retrospectively investigate the incidence, mitigating factors or importance of this event. Transient, seemingly unimportant events such as an arrhythmia, hypoxia, hypoglycemia, elevation or reduction in body temperature, leukocytosis or change in the basic metabolic profile go unrecorded unless they progress into an event that requires a major change in patient treatment. I think adverse events occurring during or after an interventional procedure should be rigorously recorded so that we can use this knowledge to improve patient care.
If you had a wish-list on three areas you could improve in IR practice, what would they be?
- Improve room turnaround time
- Better organisation of patient scheduling and follow-up
- More accurate and timely procedural recording and dissemination
What are the honors that you have received that you look back on with pride?
- Appointed to Fellowship in the Society of Interventional Radiology 1990
- Appointed to Fellowship in the American college of Radiology 1997
- Received the Barromean Medal for Distinguished Achievement 4 November 2008 from the Saint Charles Preparatory School, Columbus, Ohio where I graduated from in 1957
- Scheduled to receive The Society of Interventional Radiology 2012 Gold Medal on 27 March 2012
If you had three sentences to describe interventional radiology to someone who knew nothing about it, how would you do so?
I am not sure that my wife or children who have lived with it for over 40 years really know what interventional radiology is. Interventional radiologists have developed a paranoia concerning the image and identification of their subspecialty. Try to define surgery to an alien from Mars and you will find that it is so diverse that any definition seems inaccurate or inadequate. But, we know what surgery is, and think we know what a surgeon does; in another two or three thousand years everyone will think they know what an interventional radiologist is and does. Having voiced my disclaimer let me try: “Interventional radiology is the branch of medicine concerned with treatment of injuries or disorders of the body by incision or manipulation under the visualisation and direction of imaging modalities such as fluoroscopy, ultrasound, computerised tomography, magnetic resonance imaging or radioscintography. It usually causes less trauma to the body and organ surfaces than conventional surgical procedures and is associated with faster and less debilitating recovery.”
Which new techniques and technologies will you be watching closely in the future?
Radiofrequency ablation of the renal sympathetic nervous system; focused ultrasound; directing interventions using fusion of images from diverse imaging modalities; the efficacy of treating venous stenoses in patients with multiple sclerosis; combining two or more modalities for better cancer therapy; the injection of stem cells.











