Patients who received minimally invasive treatment with yttrium-90 (Y-90) radioactive beads to treat colorectal cancer that had spread to the liver lived almost a year longer compared to those who received the standard of care therapy, data presented at the 5th annual Symposium on Clinical Interventional Oncology, in collaboration with the International Symposium on Endovascular Therapy (ISET) has suggested.
Researchers also determined that the Y-90 treatment was more successful in patients who had not been treated with bevacizumab (standard of care biologic therapy) for at least three months prior to radioembolization therapy.
“Patients with liver-dominant metastases from colorectal cancer should be offered radioembolization in addition to chemotherapy because it may offer a survival benefit compared with chemotherapy alone,” said Dmitry Goldin, a radiology resident at Beaumont Hospital, Royal Oak, Michigan, USA, and lead author of the study.
In the study, 39 patients underwent Y-90 radioembolization, 30 of whom had also received treatment with bevacizumab. Radioembolization patients who received treatment with bevacizumab within the previous three months had a median survival of 30.5 months after diagnosis with metastatic colorectal cancer but those who had either not received bevacizumab or had been treated more than three months previously had a median survival of 37.9 months, although the difference was not statistically significant. Taking into account all the study subjects, survival averaged about 11 to 12 months longer than historical survival estimates among patients who receive standard of care treatment with modern chemotherapy and biologics alone.
Bevacizumab reduces arterial capacity. Patients who had received bevacizumab within three months of radioembolization were more likely to have therapy stopped early due to slow blood flow. This resulted in delivering less of the prescribed radiation to the tumours.
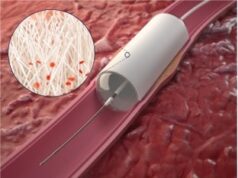
[Image: “A hepatic arteriogram from the presentation in a patient about to undergo radioembolization for metastatic liver-dominant colorectal cancer. This is a patient that never received bevacizumab and demonstrates a normal-sized proper hepatic artery and normal hepatic arterial distribution and caliber distally. This is unlike patients who received resent treatment with bevacizumab which demonstrate small and pruned hepatic arteries,” said Goldin.]