Frostbite injuries are seen at an increasing rate, and there is an increasing body of evidence supporting the use of thrombolytic therapy for its management, Ivan Babin and colleagues from Upstate Medical University, State University of New York, USA, told delegates at the International Symposium on Endovascular Therapy (ISET, 6–10 February, Hollywood, USA).
The investigators urged interventional radiologists to become familiar with the current management of frostbite injury and emphasised that they should play a critical role in the multidisciplinary special trauma team to minimise final tissue loss and maximise functionality of limbs affected by frostbite.
Babin and colleagues noted that although historically frostbite injuries were predominantly seen with military work, the last two decades had witnessed a rise in civilian cases, usually associated with winter sports, homelessness, and alcohol consumption. “Severe frostbite frequently results in ischaemia with devastating tissue injury leading to limb amputation,” Babin said.
The researchers further noted that there is a paucity of double-blind randomised trial data and grade one evidence on which recommendations are based regarding the treatment of frostbite injury. “However, the last decade has presented a growing body of evidence supporting the use of thrombolytic therapy which has led to a decrease in amputation rates,” Babin explained.
At ISET, Babin presented a comprehensive review of current management of frostbite injury and what every endovascular specialist needs to know when evaluating and treating frostbite injury. They also presented a case of successful revascularisation following catheter-directed intra-arterial thrombolyis in a 20-year-old male who suffered third-degree upper extremity frostbite injury and discussed the indications, techniques, and potential complications of this interventional radiological approach.
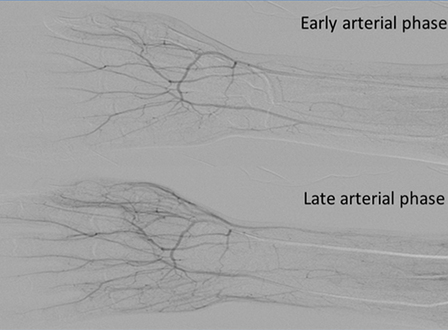
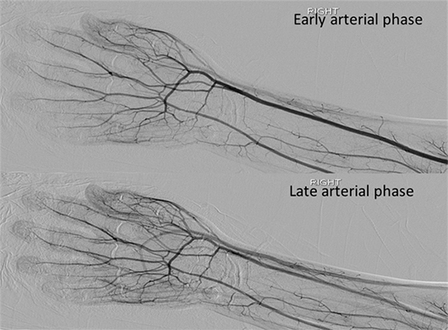
In this case, an angiogram of the right upper extremity demonstrated severe hypoperfusion of the right third, fourth and fifth digits. Following infusion catheter placement within the distal ulnar artery and a 24-hour infusion of tissue plasminogen activator and heparin, follow-up imaging demonstrated complete reperfusion of all digits. The need for surgical amputation was avoided without procedure-related complications. At one-month clinical follow-up, the patient demonstrated complete return of function and full range of motion of all digits, Babin noted.