Oncolytic immunotherapy or virotherapy is not a threat to interventional oncology—on the contrary it is a “huge and urgent” opportunity, said Daniel Sze while delivering the GEST USA Honorary Lecture. He spoke on the topic “Oncolytic virotherapy: A new class of agents to treat cancer.”
“The safety and efficacy of these biological agents depends on the mode of administration, and interventional radiologists are uniquely qualified to deliver these agents,” added Sze, professor of Radiology, Stanford University, USA, at the Global Embolization Symposium and Technology (GEST USA, 5–8, May, New York, USA).
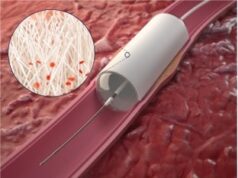
“If a virus is administered intravenously, which is how medical oncologists like to administer agents, some of it sticks to the vessel wall; some of it is inactivated by complement; some is neutralised by circulating antibodies. Then, some of it sticks to blood cells and to the heart and lungs, and some of it is taken up by the reticuloendothelial system, even before it gets into the arteries feeding the tumour. Once it gets there, it can stick to the stroma and can be repelled by the high oncotic pressure in the tumour. We, in interventional radiology, can bypass almost all of these things. We can inject the virus into the tumour-feeding arteries and not cause toxicity to the other organs. We can also directly inject into the tumour to bypass the stroma and high pressure. We are the virus whisperers. Oncolytic virotherapy needs interventional radiology,” he explained.
As described by Stephen J Russel and colleagues in Nature Biochemistry in 2012: “Oncolytic virotherapy is an emerging treatment modality that uses replication-competent viruses to destroy cancers. Recent advances include preclinical proof of feasibility for a single-shot virotherapy cure, identification of drugs that accelerate intratumoural virus propagation, strategies to maximise the immunotherapeutic action of oncolytic viruses and clinical confirmation of a critical viremic threshold for vascular delivery and intratumoural virus replication.”
Russel and colleagues further go on to add: Key challenges for the field are to select ’winners’ from a burgeoning number of oncolytic platforms and engineered derivatives, to transiently suppress but then unleash the power of the immune system to maximise both virus spread and anticancer immunity, to develop more meaningful preclinical virotherapy models and to manufacture viruses with significantly higher yields than is currently possible.
In his lecture, Sze stated that he preferred the term “immunotherapy” over “virotherapy,” since the latter may be scary to the public. After thanking the organisers for allowing him to “get on my soapbox to preach about the benefits of viruses, even though they are not embolic agents,” Sze went on to outline that there have been many years of historical reports of viruses suppressing cancer.
According to Sze, as early as 1904 (when it was still unknown that viruses caused influenza), George Dock, a physician, published a report on a woman who experienced remission from myelogenous leukaemia after suffering an upper respiratory infection, now presumed to be influenza. Since there was no imaging available at the time, Dock drew anatomical images of palpated organ size showing splenomegaly and hepatomegaly that both resolved after the influenza attack. In 1912, De Pace reported that a cervical cancer patient became cancer-free after being bitten by a rabid dog. The patient was given a rabies vaccine to prevent her from contracting the disease and a few weeks after this, De Pace reported that the tumour had disappeared. Subsequently, in 1923, Romanian physicians Lavditi and Nicolau wrote: “Tumours are more susceptible to viruses than normal cells, and tumours act as a sponge attracting viral replication.” In the 1940s, wild type murine viruses that were given intravenously to mice succeeded in suppressing tumours, but there was also so much toxicity from the viruses themselves that the mice died.
In the 1940s and 1950s, the first human clinical trials were run, but since there were no options for genetic engineering at the time, various wild type viruses including the Hepatitis B virus and West Nile virus were used. These were collected in the form of serum from a diseased person, and then injected intravenously, intratumourally, intramuscularly, intra-arterially, or inhaled. As would be expected, there was often severe toxicity, such as fulminant hepatitis or encephalitis, and this aspect put the kibosh on trials of this kind, noted Sze.
In the 1970s, the development of recombinant DNA technology resulted in the ability to engineer viruses, which led to a revival of the field. Engineered viruses have been in human trials since 1996 and in 2005, Sunway Biotech received Chinese FDA approval for Oncorine, a recombinant human adenovirus used to treat head and neck cancers. Oncorine only garnered a very small market, mainly because it was not covered by Chinese national health insurance. By 2014, there were more trials listed on ClinicalTrials.gov on oncolytic virotherapy than on gene insertion cancer gene therapy. In October 2015, the first oncolytic virus was approved by the US FDA, to treat late stage melanoma by direct skin lesion injection.
The expanding interest in the field has occurred because the viruses can now be engineered to be more specific, more safe and more effective, which means they can behave as biological smartbombs, destroying just their target, but not their surroundings. However, they must still be handled by experts, cautioned Sze.
How does oncolytic immunotherapy work?
Normal cells are usually not susceptible to viral infection, having their own biochemical methods of recognising viral infection and shutting them down. However, cancer cells have abnormal mechanisms for recognising and eliminating abnormal DNA (ie the viruses or the cancer mutations). So the viruses can selectively infect the cancer cells and replicate inside so that eventually that cancer cell is overblown with the virus particles, leading to cell lysis. This releases new viral particles that infect the neighbouring cancer cells and also release new tumour antigens that can be recognised by the human immune system.
Interestingly, said Sze, oncolytic immunotherapy can work by immunomodulation to cause an “abscopal” effect or systemic response, and this is important, particularly because most oncologists still view cancer as a systemic disease. Now, a locoregional treatment can produce a systemic effect, and this can be used to help convince dogmatic oncologists of the validity of the therapy, he noted.
The evolution of radiographic response criteria
At the GEST USA meeting, Sze stated that oncolytic virotherapy demands new standards of radiographic response. “In terms of radiographic response evaluation, the early results (of clinical trials) were very disappointing and there was a high rate of tumour enlargement even within one month. However, these findings were discordant with improvements in tumour marker levels and clinical health. We often saw tumours getting bigger after treatment, before they got smaller, in a phenomenon now called “pseudo-progression.” It is now increasingly accepted that WHO and RECIST criteria are not representative of response for biologic agents, radiofrequency ablation, transarterial chemoembolization, radioembolization, etc, and there are several new standard modifications to these including irRECIST, which are “immune-related” criteria for response,” Sze said.
Trials
There are several new oncolytic immunotherapy clinical trials involving interventional radiology, including the T-VEC (Amgen) phase I trial treating hepatocellular carcinoma or liver metastases using intratumoural injection of the oncolytic virus T-VEC, using ultrasound or CT guidance. T-VEC, under the brand name Imlygic, was the agent approved by the US FDA in October 2015 for treatment of late stage cutaneous melanoma. In March, SillaJen announced that the first US patient was enrolled in the ongoing multinational randomised phase III open-label study of Pexa-Vec (formerly Jennerex, JX-594), in patients with advanced hepatocellular carcinoma. The trial is evaluating the use of Pexa-Vec to treat hepatocellular carcinoma patients who have failed locoregional therapies and are eligible for treatment with sorafenib.
Named the PHOCUS trial, the study is designed to enroll 600 patients who have not received prior systemic treatment for their cancer, who will be randomised to sorafenib with or without Pexa-Vec. The study will be conducted at approximately 140 sites worldwide including North America, Asia, Australia, and Europe.
“Oncolytic virotherapy is a form of biological warfare against cancer that involves exploiting existing pathogens and engineering or tailoring them to suit our needs. Their mechanism of action is profoundly different from other treatment options, and involves oncolysis and immunomodulation. The science and regulation surrounding these agents is extremely complex, but the expertise of the interventional radiology community will be crucial for its success,” Sze concluded.