This advertorial is sponsored by Merit Medical.
Disclaimer: The suggestions and other information, which may include both Merit and third-party products, are for the practitioner’s convenience and for general information purposes only. This information does not constitute medical or legal advice, nor is it meant to endorse or guarantee the suitability of any of the referenced products or methods for any specific patient or procedure. Before using, refer to the instructions for use (IFU) for indications, contraindications, warnings, precautions, and directions for use.
Before using any product, refer to the IFU for indications, contraindications, warnings, precautions, and directions for use.
Pavan Najran (The Christie Hospital NHS Foundation Trust, Manchester, UK), clinical lead for interventional radiology (IR) and consultant clinical and interventional radiologist, explores solutions for gaining access and management in the distal radial route specifically within interventional oncology setting.
The transition from femoral to radial access intervention has been supported by favourable evidence demonstrating improved mortality and morbidity outcomes1. In addition to this, radial access has been shown to be favourable to patients, a preference that has been supported by numerous studies2 which reference considerable patient data.
Traditional radial access has limitations, including ergonomics and patient positioning, which become apparent during longer procedures.
Distal radial access was first performed and reported in 20173 by Ferdinand Kiemeneij (Onze Lieve Vrouwe Gasthuis, Amsterdam, The Netherlands) et al and has since been adopted by both the cardiology and radiology groups. In the setting of interventional oncology, radial access offers significant benefits, particularly when performing prolonged procedures in patients with deranged clotting function, a group of patients commonly encountered in this setting.
How to anatomically navigate distal radial access
The anatomical snuff box houses the distal radial artery, a distal branch of the main radial artery, and as a result any occlusion of the vessel locally is less likely to compromise blood supply to the hand, adding to its advantage.
The anatomical snuff box is a depression at the base of the thumb. It is bordered by the extensor polices longus medially and the abductor polices longus, as well as the extensor pollicis brevis laterally. These structures can be identified easily when the thumb is fully extended.
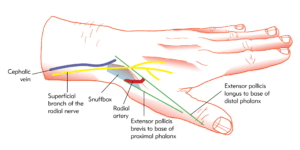
The vessel is punctured distal to the superficial palmer branch and proximal from the pollicis brevis artery.
Distal radial access and ultrasound techniques
Advantage of a distal approach is that the access arm can be moved into various positions given the position of the hand at puncture, even allowing for left arm access from a right sided patient position.
The technique used for traditional radial access can be translated into distal techniques, however there are a number of points that require consideration.
The hand can be placed in a more natural position for the patient, with the thumb pointing towards the celling. Traditional radial access requires the palm surface of the hand to be facing the ceiling, which can become uncomfortable during prolonged procedures.

Ultrasound guided access is a must due to the marginal reduction in vessel diameter and close abutment of the adjacent tendons. A high-frequency probe with a small footprint is recommended due to the smaller surface contact; a musculoskeletal (MSK)-based hockey stick probe is recommended if available.
Managing distal radial access
Enable easier puncture, supporting a selection of sheath sizes and reduce risk of spasm.
A combination local anaesthetic and glyceryl trinitrate (GTN) (9ml of 1% lignocaine + 200mcg GTN) should then be infiltrated around the vessel carefully ensuring the vessel is bathed in the medication extending from the desired puncture site, proximally to the main radial artery. The local anaesthetic will provide the necessary analgesia, and the GTN will dilate the vessel; this will make the puncture easier and ensure that larger sheath sizes can be placed without difficulty. Further to this, proximal GTN and anaesthetic infiltration will ensure the main radial trunk is dilated and therefore reduces the risk of spasm as the sheath is inserted.
A 21-gauge needle is then used to puncture the vessel, which should be performed under ultrasound guidance in a transverse plane—this ensures the vessel is punctured in the 12 O’clock position reducing the risk of sub-intimal cannulation. An intraluminal puncture should produce prominent blood flow from the needle. Furthermore, a 0.018 guidewire should then be placed through the needle intraluminally. If there is any resistance to the wire insertion, a sub-intimal or side branch location is likely, so readjustment is required. A confirmatory ultrasound can then be performed ensuring an intraluminal location.
The sheath can then be inserted, a skin incision should not be performed as the traction from the skin will prevent the sheath from falling out. Again, a confirmatory ultrasound can be performed, ensuring an intraluminal location. Once in place, a cocktail of heparin (5000iu) and GTN (200mcg) should be instilled through the sidearm. Calcium channel blockers (verapamil 2.5mg) can also be used within the cocktail however, this should be used with caution, as if the patient is currently on antihypertensives, this can result in sudden hypotension.
Once the sheath is in place, access into the leading vessel is achieved via the catheter inserted into the sheath and a hydrophilic wire preloaded within it, allowing negotiation through to the aortic arch under fluoroscopic guidance.
Once the aortic arch is negotiated the catheter of choice is based on the target vessel. Pelvic vessels may favour a less aggressive angled tip catheter, whereas coeliac access intervention may require a more exaggerated angled catheter.
References
- Chiarito M, Cao D, Nicolas J, Roumeliotis A, Power D, Chandiramani R, Sartori S, Camaj A, Goel R, Claessen BE, Stefanini GG, Mehran R, Dangas G. Radial versus femoral access for coronary interventions: An updated systematic review and meta-analysis of randomized trials. Catheter Cardiovasc Interv. 2021 Jun 1;97(7):1387–1396. doi: 10.1002/ccd.29486. Epub 2021 Jan 28. PMID: 33507598.
- Satti SR, Vance AZ, Golwala SN, Eden T. Patient Preference for Transradial Access over Transfemoral Access for Cerebrovascular Procedures. J Vasc Interv Neurol. 2017 Jun;9(4):1–5. PMID: 28702112; PMCID: PMC5501120.
- Left distal transradial access in the anatomical snuffbox for coronary angiography (ldTRA) and interventions (ldTRI) Kiemeneij F.EuroIntervention.2017;13:851–857.









