Percutaneous intra-articular pulsed radiofrequency neurolysis seems to be an effective and safe technique in the palliative management of chronic pain in patients with knee osteoarthritis, found research presented at the Society of Interventional Radiology annual scientific meeting in Vancouver, earlier this year.
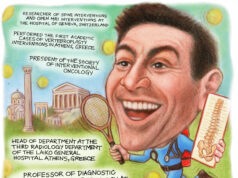
Dimitrios K Filippiadis (assistant professor of Diagnostic and Interventional Radiology) and Alexis Kelekis (associate professor of Diagnostic and Interventional Radiology), in the 2nd Radiology Department, University General Hospital “Attikon”, Medical School National and Kapodistrian University of Athens, Greece, set out to prospectively evaluate the effectiveness of percutaneous imaging-guided intra-articular pulsed radiofrequency neurolysis in patients with knee osteoarthritis suffering from chronic pain refractory to conservative therapies.

“Patients included in our study were suffering from symptomatic, advanced knee osteoarthritis diagnosed with X-rays and classified as grade III or IV according the Kellgren–Lawrence classification. All patients had undergone some kind of conservative treatment in the past six months including analgesics and nonsteroidal anti-inflammatory drugs as well as physiotherapy, without any recorded benefit,” Filippiadis told Interventional News.
Commenting on the researchers’ hypothesis about the mechanism of action of pulsed neurolysis, Filippiadis noted: “In large joints such as the knee, intra-articular application of pulsed radiofrequency works in two ways. First, it suppresses the excitatory C-fibre response and the synaptic transmission, thus influencing the nervous system and providing immediate pain relief. Additionally, it influences the immune system and inhibits production of proinflammatory cytokines, such as interleukin-1b and interleukin-6 by immune cells affecting inter-cellular communication.”

The investigators used intra-articular pulsed radiofrequency neurolysis to treat 40 cases of knee osteoarthritis in the last year. With regard to the procedure, they inserted a 20G/10cm cannula percutaneously in the anterolateral region of the knee joint under fluoroscopy. Then, a radiofrequency electrode with a 10mm ‘‘active tip’’ was coaxially introduced and a 10-minute neurolysis session was performed using pulsed radiofrequency. The patients were then treated with an intra-articular injection of hyaluronate. The researchers measured pain before the procedure, at one week after the procedure, and at one and six months after the procedure. These records were then compared by means of a numeric visual scale (NVS) questionnaire.
Filippiadis and colleagues found that there was decreased pain and improved quality of life at one week, one month and six months after the procedure when compared to scores obtained prior to the procedure.
“Overall mobility improved in 38/40 (95%) of patients and there were no complications observed with the procedure. The results seem to be reproducible and appear to last longer than if intra-articular injection of hyaluronate alone is administered,” Filippiadis said.
Commenting further, he noted that the enrolment in this study is now closed. “We have enrolled 40 consecutive patients who underwent intra-articular pulsed radiofrequency neurolysis and are following them with phone calls and clinical visits for one year. Our final results including the pain scores at one-year follow-up will be presented at CIRSE 2016 on 11 September,” he said.