In the United States, more than 100,000 amputations are performed each year on individuals with critical limb ischaemia, the most severe form of peripheral arterial disease. The number one priority in treating these patients is to re-establish blood flow to avoid limb amputation. Interventional radiologists have found that a subgroup of patients with critical limb ischaemia may avoid amputation through the use of drug-eluting stents on the smaller arteries below the knee, according to a study released at the Society of Interventional Radiology’s Annual Scientific Meeting in Tampa, USA.
Drug-eluting stents are an emerging technology that offers hope to peripheral arterial disease patients with critical limb ischaemia and freedom from major amputations. The placement of drug-eluting stents in the infrapopliteal leg arteries is safe and effective and can significantly impact their care. Our results rival bypass surgery and are better than balloon angioplasty alone,” said Robert A Lookstein, an interventional radiologist and associate director of the division of interventional radiology at Mount Sinai Medical Center in New York, USA. Primary patency for the 53-patient study at 12 months was 81.8% (45/55), said Lookstein, who is also an associate professor of radiology and surgery at Mount Sinai School of Medicine. Freedom from major amputation at follow-up was 90.6% (48/53) for the entire group and 100% (44/44) for patients with Rutherford category 4 (ischaemic pain at rest) and 5 (lower-extremity ischaemia associated with minor tissue loss) disease.
The Rutherford categories are a severity classification scale for peripheral arterial disease that can be used to evaluate clinical improvement. Patients were followed for an average of 17 months.
“Currently patient follow-up out to 24 months is incomplete and will be finalised by the end of the year,” Lookstein said.
Late in 2009, preliminary results from the DESTINY trial showed that at six-month follow-up, drug-eluting stents had a higher primary patency rate in below-the-knee critical limb ischaemia lesions compared to bare metal stents. This provoked the question of whether the awaited 12-month angiographic results will confirm the benefits of drug-eluting stents or whether there would be a setback for drug-elution.
Several researchers have been spurred on by the initially promising results of sirolimus-eluting stents in the coronary arteries and have applied them in the infrapopliteal arteries in order to fight restenosis and prolong amputation.
Recently published data from controlled trials of sirolimus-eluting stents have shown favourable results at six and 12 months, with superior angiographic patency and fewer re-interventions compared to bare metal stents.
Siablis et al have carried out a non-randomised prospective single-centre study comparing sirolimus-eluting to bare metal stents in 29 patients with critical limb ischaemia assigned to each study arm (65 bare vs. 66 sirolimus-eluting stents) after suboptimal angioplasty or flow-limiting dissection. Six-month results have shown that sirolimus-eluting stents had significantly higher primary patency and decreased in-stent binary restenosis. Results of this study at one year have proved to be just as optimistic, showing superior primary patency and less in-stent restenosis.
The investigators reported no significant differences between the sirolimus-eluting and bare metal stent groups with respect to one-year mortality, minor amputation, and limb salvage, but the rate of target lesion revascularisation was significantly less in the sirolimus-eluting stent group, both at six months and one year.
Siablis et al also recently reported long-term outcomes from an extended study with more than 100 patients. In this study, follow-up out to three years, showed that sirolimus-eluting stents were associated with significantly higher primary patency and improved target lesion revascularisation-free survival compared to bare metal stents.
Similarly, Scheinert et al have found in a non-randomised single centre study that primary sirolimus-eluting stent placement is more effective than bare stents for select infrapopliteal lesions. The study enrolled 60 patients, the majority of whom had critical limb ischaemia. Patients were treated with either sirolimus-eluting or bare metal stents. At six months, restenosis and target lesion revascularisation were much lower in the sirolimus-eluting stent group. Overall limb salvage was not remarkably different between the two study groups.
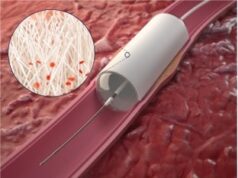
Surgical bypass remains the mainstream therapy for tiny blocked infrapopliteal arteries, but there are a growing number of patients who are unable to undergo this treatment because of their medical problems, said Lookstein. Attempts to treat critical limb ischaemia in peripheral arterial disease patients with below-the-knee angioplasty are hindered by high rates of restenosis, the need for repeat treatments and the continued progression of atherosclerotic disease. Drug-eluting stents are a potential solution to the limitations of endovascular treatment. An interventional radiologist performs a balloon angioplasty to open a narrowed blood vessel and then places a drug-eluting stent in that artery. The stent acts as scaffolding to hold the narrowed artery open. Drug-eluting stents slowly release a drug for several weeks to block cell proliferation and regrowth, thus inhibiting restenosis.
Over a four-year period, Lookstein’s group at Mount Sinai Medical Center in New York studied 53 patients (32 men, 21 women) ranging in age from 43 to 93 who underwent implantation of 94 drug-eluting stents (80 sirolimus, 12 evirolimus, two paclitaxel) to treat a suboptimal angioplasty result in an infrapopliteal artery. All patients had symptoms of critical limb ischaemia with Rutherford grade 4 (15), 5 (29) or 6 (9) disease at presentation prior to treatment. Initial technical success rate was 100% with all treated lesions having less than 10% residual angiographic stenosis at completion of the procedure. The mean number of stents placed per patient was 1.62 (range, 1–5), with the stent diameter ranging from 2.5 to 4mm. Angiographic, clinical and noninvasive vascular examination results were collected prospectively at regular intervals. Primary endpoints, including technical success of the revascularisation procedure, primary patency, freedom from major amputation and survival at follow-up, rival those of conventional bypass surgery.
“Our study reinforces the fact that when it comes to treating cardiovascular disease, there is a wide range of safe and effective treatments,” said Lookstein. Multicentre, randomised trials are necessary to support such promising results of the value of infrapopliteal drug-eluting stents in critical limb ischaemia treatments, he added.
In the USA, drug-eluting stents are FDA-approved for the coronary arteries but not for infrapopliteal arteries.