The incidence of lung cancer has increased considerably in the last few decades with the lung as the most common site of metastatic involvement. Despite the improvements in the diagnosis and treatment for malignant lung tumours, the prognosis of the patients is still unsatisfactory.1 Currently, locoregional chemotherapeutic techniques such as transpulmonary chemoembolization (TPCE) for the treatment of lung malignancies have gained increasing importance. The purpose of this retrospective study was to evaluate local tumour response and patient survival after the treatment of pulmonary metastases using TPCE as a palliative treatment method.
In TPCE, a 5 French (Fr) endovascular sheath and 5Fr headhunter catheter are routinely placed transfemorally under fluoroscopy until the pulmonary artery and subsequently the tumour-feeding segmental pulmonary branch are reached. A balloon catheter (up to 7mm in diameter) is optionally placed for better results.2 This selective pulmonary artery catheterisation results in a blockage of the arterial supply to the tumour tissue, resulting in regional ischaemic necrosis in the target tumour tissues while reducing damage to the surrounding normal lung parenchyma. Thereafter, mitomycin and gemcitabine as chemotherapeutic agents are administered in combination with an embolization of lipiodol and microspheres. This extends the storage time of the injected cytostatics in the tumours and reduces the outflow into the circulatory system.3 Consequently, the frequency and severity of systemic effects are limited. Other occlusion materials used are coils, polyvinyl alcohol, degradable starch microspheres, and gelatin sponges.
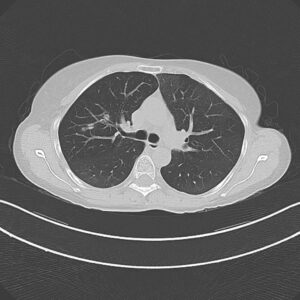
In our study, 223 patients (138 women, 85 men; mean age: 59.3±11.9 years) with unresectable lung metastases and/or not responding to systemic chemotherapy received repetitive TPCE (mean number of sessions 4.7±3.7) between January 1990 and May 2021. Patients had predominant lung metastases and in most cases with bilateral lung involvement. Origin of the metastases were either colorectal carcinoma (n=139) or breast cancer (n=84). Tumour-supplying vessels were catheterised selectively in order to apply chemotherapeutic agents locally, combined with lipiodol and microspheres. The response was assessed according to the revised RECIST criteria.
Of the evaluated 183 cases, partial response was achieved in 4.9% (n=9), stable disease in 62.3% (n=114), and progressive disease in 32.8% (n=60) of the patients. Mean and median overall survival time were 23.5 and 14 months, respectively.
TPCE can be used as a palliative treatment in unresectable lung malignancies to reduce the tumour burden or to achieve local tumour control,4 or as a neoadjuvant or curative treatment option combined with thermal ablation such as radiofrequency ablation (RFA) and microwave ablation (MWA) (Figure 1).5,6


A multicentre study may include a larger population of patients and combine expertise from different institutes. Although TPCE has the potential to improve local tumour control and to prolong survival, randomised controlled trials are still needed.
Thomas Vogl is director of the Institute for Diagnostic and Interventional Radiology at University Hospital Frankfurt (Frankfurt, Germany).
Disclosures: The author shared no relevant disclosures
References:
- Lemjabbar-Alaoui H, Hassan OU, Yang Y-W et al. Lung cancer: Biology and treatment options. Biochim Biophys Acta 2015; 1856: 189-210.
- Vogl, TJ, Herzog C, Zangos S, Lindemayr S. Transpulmonale Chemoembolisation (TPCE) als palliatives Behandlungskonzept bei primären Lungentumoren. Fortschr Rçntgenstr 2007; 179: 300-307
- Vogl TJ, Mekkawy AIA, Thabet DB, et al. Transvenous pulmonary chemoembolization (TPCE) for palliative or neoadjuvant treatment of lung metastases. Eur Radiol 2019, 29: 1939-1949
- Vogl TJ, Shafinaderi M, Zangos S et al. Regional chemotherapy of the lung: transpulmonary chemoembolization in malignant lung tumors. Semin Interven Radiol 2013; 30: 176-184
- Smith SL, Jennings PE. Lung radiofrequency and microwave ablation: A review of indications, techniques and post-procedural imaging appearances. Br J Radiol 2015; 88, 20140598
- Vogl TJ, Hammann L, Adwan H. Transvenous Pulmonary Chemoembolization and Optional Microwave Ablation for Colorectal Lung Metastases. J Clin Med 2023; 12(10):3394