As a world-leading advocate of the “emborrhoid” technique—the embolization of the superior rectal arteries—and the lead author of the 2015 study demonstrating the procedure’s efficacy, Vincent Vidal provides an update four years on concerning the current status of the technique. In 1994 and 1998, EV Galkin (Krasnoyarsk, Russia) first described a potential interventional radiology treatment for chronic haemorrhoids complicated by haemorrhage. Published in Russian, the audience for these two papers was limited, and Vidal has been a pioneer for the furtherance of this work outside of Russia. With a randomised, comparative evaluation of the emborrhoid technique underway, Vidal hopes to confirm its place as a minimally-invasive, therapeutic alternative for treating patients with haemorrhoidal disease.
With a prevalence of 4–35%, haemorrhoidal disease is the most common anorectal condition. One of the main chronic symptoms is rectal bleeding. Its recurrence can alter the quality of life and, more rarely, cause anaemia. Pain is less common, only occurring in the event of a complication (congestive exacerbation, external haemorrhoidal thrombosis, fissures). The most common treatment involves hygiene and dietary measures, phlebotonics and/or nonsurgical outpatient treatment (infrared photocoagulation, elastic band ligation).
The haemorrhoidal arteriovenous network is a normal vascular formation. Internal haemorrhoids are now thought to result from an increase in arterial blood flow from the rectal arteries into the haemorrhoidal cushion (corpus cavernosum recti).1 Expansion of the vascular network of the anorectal submucosa initiates a negative vicious circle of progressive vascular dilation and venous insufficiency, leading to haemorrhoidal hyperplasia. This hyperplasia causes an increase in blood pressure, arterial inflow and anal pressure in the corpus cavernosum recti. The mechanical function of the corpus cavernosum recti is dependent on the influx of arterial blood from the branches of the inferior mesenteric artery, the superior rectal arteries, but also in 30 to 50% of patients from the unilateral or bilateral middle rectal artery. By contrast, the lower part of the rectum and the anal canal are supplied with blood by the inferior and middle rectal arteries, both of which have origins at some distance from the inferior mesenteric artery (pudendal artery, iliac network).2
Ten years ago, proctologists developed a new concept of treatment: elective transanal Doppler-guided haemorrhoidal artery ligation (DGHAL). The DG-HAL technique involves the identification and ligation of the superior rectal arteries under transanal Doppler guidance. Ligation of the superior rectal arteries provides a significant reduction of arterial blood flow to the haemorrhoids, and is effective in treating haemorrhoid disease.3
We have suggested that arterial ligation can be performed with coils in the terminal branches of the superior and middle rectal arteries via the endovascular route.
The advantages of emborrhoid and DG-HAL technique versus surgery are that it maintains the haemorrhoidal tissue in place, preserves anal continence, has no rectal wounds (meaning no local care is necessary), there is significantly less pain, and the complications of open surgery are avoided, thus allowing a faster return to activity.
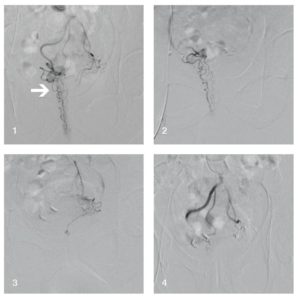
Emborrhoid embolization is performed using a right femoral route. The inferior mesenteric artery is catheterised using a Simmons or Sidewinder catheter. The superior rectal arteries are then catheterised with a microcatheter. Coils used for the embolization are 0.018’’, from 2–3mm in diameter. Distal opacification of the superior rectal artery may depict a direct anastomosis with a dominant middle rectal artery in 30 to 50% of cases. In this situation, the middle rectal artery should be also embolized after catheterisation of the anterior trunk of the hypogastric artery.
The technical success of the emborrhoid technique has been reported to be up to 90%. Meanwhile, the clinical success is also impressive: the literature reports between 74 and 83% of patients treated with the emborrhoid technique as having no complications.2,6
The main advantages of emborrhoid technique are:
- Patients have absolutely no pain.
- No major complications have been related to the emborrhoid technique, and especially no ischaemic or continence complications.
- This technique is available in an outpatient setting.
- The patient can return to activity the day after embolization.
- Embolization does not close the door to a complementary treatment if mandatory.
- The technique is easy to perform in an hour or less, especially if there is no need for middle rectal artery embolization.
There are many benefits of endovascular treatment, including the complete visualisation of all the branches of the superior rectal arteries and anastomoses with middle and inferior rectal arteries.7 With the DG-HAL technique, it is possible that not all arteries are detected, which can lead to incomplete treatment, especially if there are anastomoses. Obviously, embolization eliminates the risk of direct anorectal trauma. There are many patients who suffer from haemorrhoids but do not complain to physicians because they refuse to have an endorectal treatment. If we can offer a treatment for outpatients without pain, we believe more patients will seek treatment for this condition.

We have demonstrated that distal coil embolization of the superior and middle rectal arteries to stop chronic bleeding is safe and effective. Many clinical studies are ongoing in Europe, Asia and America. We are now building a randomised, comparative evaluation with DG-HAL to confirm the role of the emborrhoid technique as a minimally invasive therapeutic alternative for haemorrhoidal disease.
Vincent Vidal is the head of the Interventional Radiology section in the Department of Medical Imaging at the University Hospital TIMONE in Marseilles, France.
References
1. Aigner F, Bodner G, Conrad F, Mbaka G, Kreczy A, Fritsch H. The superior rectal artery and its branching pattern with regard to its clinical influence on ligation techniques for internal hemorrhoids. Am J Surg 2004; 187:102–108
2. Moussa N, Sielezneff I, Sapoval M, Tradi F, et al. Embolization of the superior rectal arteries for chronic bleeding due to hemorrhoidal disease. Colorectal Dis. 2016 Jun 24. doi: 10.1111/codi.13430.
3. Infantino A, Altomare DF, Bottini C et al. Prospective randomized multicentre study comparing stapler haemorrhoidopexy with Doppler-guided transanal haemorrhoid dearterialization for third-degree haemorrhoids. Colorectal Dis 2012; 14:205–211
4. Vidal V, Louis G, Bartoli JM, Sielezneff Y. Embolization of the hemorrhoidal arteries (the emborrhoid technique): a new concept and challenge for interventional radiology. Diagn Interv Imaging 2014 95:307–315
5. Vidal V, Sapoval M, Sielezneff Y, De Parades V, Tradi F, Louis G, Bartoli JM, Pellerin O. Emborrhoid: a new concept for the treatment of hemorrhoids with arterial embolization: the first 14 cases. Cardiovasc Intervent Radiol 2015; 38:72–8
6. X. Sun a, y, J. Xub, y, J. Zhang a, Y. Jina, Q. Chen. Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: a single-centre experience and protocol. Clinical Radiology 2018; 73:985.e1-6.
7. Bilhim T, Pereira JA, Rio Tinto H, et al. Middle rectal artery: myth or reality? Retrospective study with CT angiography and digital subtraction angiography. Surg Radiol Anat 2013; 35:517–522










