Evasion of the immune system is an important mechanism in the development and progression of cancers. Cancer immunotherapies are a promising class of therapeutic agents that re-engage the immune system in its fight against cancer cells, explained Vicky Goh, London, UK.
Goh was speaking at the press conference of European Congress of Radiology (ECR; 28 February–4 March, Vienna, Austria).
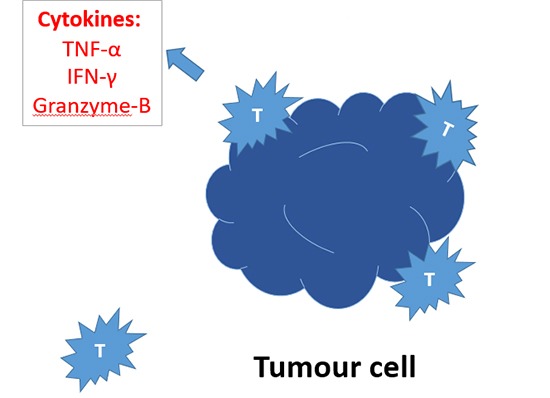
“These therapies use strategies that range from activating innate/adaptive immune effector mechanisms to neutralising inhibitory/suppressive mechanisms. For example, treatment with interleukin 2 (IL-2) or interferon-α (IFNα) stimulates effector immune cells. Conversely antibodies against immune-checkpoint molecules (eg. cytotoxic T lymphocyte-associated protein 4 [CTLA4]-targeted antibodies and programmed cell death 1 [PD1]-targeted antibodies) neutralise immune suppressor mechanisms,” said Goh, chair of Cancer Imaging and head of Department at King’s College London and honorary consultant radiologist and academic lead at the Guy’s and St Thomas’ Hospitals, London/UK.
Immunotherapies have shown to be effective in a number of advanced cancers including melanoma and non-small cell lung cancer where improvement in overall survival has been achieved. For melanoma, ipilimumab (an anticytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) antibody) was approved in 2011, based on results from a phase III trial, in which 20% of patients with melanoma experienced long-term survival. Since then nivolumab and pembrolizumab, antibodies targeting programmed cell-death protein 1 (PD-1), have been associated with response rates of 28–40%.
However, it is important to note that only 20–40% of advanced melanoma patients have durable responses to immune checkpoint inhibitors, said Goh noting that their positive effects need to be balanced against severe off-target immune toxicity and high costs.
Goh alluded to the “the good, the bad and the ugly” about this new treatment option. “The trials have shown that immunotherapies prolong overall survival, may be synergistic and their effects on tumours are different to standard chemotherapy, or targeted therapies, such as antiangiogenics. The response can be slow in onset but prolonged, and there are significant side-effects such as on the skin and gastrointestinal system, most commonly. Up to a third of patients may have to discontinue treatment,” she noted.
Future research directions
Her talk also focused on the role of imaging and considered future research directions. “Predictive biomarkers to select patients with likely clinical benefit from treatment are needed. Can imaging play a part? As immunotherapies generate anti-tumour effects by enhancing tumour-specific T cell responses rather than the direct cell killing, therapy assessment may be challenging by imaging. Response may take longer to be detectable by imaging and standard methods, such as Response Evaluation Criteria in Solid Tumours (RECIST) may be misleading,” said Goh ahead of the ECR press conference.
“The challenge for imaging is how best to assess if therapy is working, or not, given the high likelihood of treatment-related side effects. Further, how best to identify the patients who are likely to benefit from treatment; how best to exploit interventional oncology in the era of immunotherapies and the question of whether interventional oncology can harness the abscopal effect all remain research issues,” said Goh.












