Hans van Overhagen and Jim A Reekers from The Netherlands have authored the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Standard of Practice guidelines for transcatheter uterine artery embolization (UAE) for symptomatic leiomyomata and these have been published in Cardiovascular and Interventional Radiology (CVIR). The authors urge that every symptomatic patient with uterine myomas should be offered embolization as alternative treatment to hysterectomy/myomectomy. “UAE should be incorporated in the (national) gynaecological guidelines,” they report.
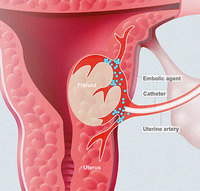
The standard of practice guidelines outline the pre-treatment imaging, indications for treatment and contraindications, patient preparation, equipment specifications, procedure, medication and peri-procedural care, post-procedural follow-up and care, outcome and effectiveness and complications associated with UAE.
The authors write that UAE is a true alternative to hysterectomy in women who want to preserve their uterus, a statement that is backed by level one evidence. Further, they find that the highest quality of evidence shows that the five-year outcome in quality of life is equal in groups treated either by hysterectomy or by UAE, with no difference in major complications. Van Overhagen and Reekers point out that level one evidence also shows that a 15–20 % hysterectomy rate has to be expected during follow-up after successful embolization and that in the short-term, UAE had lower blood loss, shorter hospital stay and quicker return to work. The authors further conclude that the risk for ovarian dysfunction after UAE seems over-estimated in women less than 40 years of age.
The indications for UAE are heavy menstrual bleeding, mechanical complaints, such as pain, pressure, dyspareunia, urinary urgency and frequency. Van Overhagen and Reekers emphasise that all possible candidates for UAE should undergo assessment by a gynaecologist with training and experience. “The examination should confirm the diagnosis of leiomyomata and exclude a viable pregnancy and/or active infection or malignancy of the vagina, cervix, uterus and ovaries. All candidates should also undergo assessment by the attending interventional radiologist in order to be informed about the procedure, clinical success rates, complications and follow-up,” they note.
The absolute contradictions to receiving UAE are pregnancy, malignancy of the uterus or ovaries (unless the procedure is being used for palliation or as an adjunct to surgery and active uterine infection. A relative contraindication is the patient desire to preserve childbearing potential. The authors make it clear that the effect of UAE on fertility has not been well investigated and that preservation of fertility is not assured from the current literature. However, uncomplicated pregnancies and normal deliveries have been reported after UAE, as also conflicting results regarding the effect of UAE on pregnancy and miscarriage rates. “Thus, this procedure may be considered for women who are not candidates for myomectomy, however, not as a first choice option,” they write.
Other anatomical features may also play a role for the procedure to be relatively contraindicated: pedunculated subserosal fibroids with thin stalks; a common arterial supply of uterus and ovaries; and the presence of intrauterine device must be taken into account (However, the authors point to a recent series of 20 women, accidentally embolized with an IUD in situ did not show any infectious side effects, level 4 evidence). General contraindications for endovascular procedures including contrast material allergy, impaired renal function and coagulopathy also apply, and these may be treated before UAE.
With regard to complications, as reported in CVIR, major complications of both hysterectomy and UAE are rare and equal in the randomised trials. “Major complications are reported in up to 5% during and within the first month of the procedure. Pulmonary embolism and deep vein thrombosis are reported in less than 1%. Transcervical expulsion of fibroid tissue, occasionally necessitating surgery in ±5% of procedures and major infection in 2.5%. There have been three reported deaths due to UAE. In randomised clinical trials, common complications are discharge and fever (4%), technical failure (4%) and post-embolization syndrome (3%). Amenorrhea is reported in ±4% of women, permanent in less than 2%,” the authors write.