 The Auryon atherectomy system (AngioDynamics) “represents an exciting new technology”, John Rundback (Advanced Interventional and Vascular Services, LLP, Teaneck, USA) opined at the International Symposium on Endovascular Therapies (ISET; 9–11 May, Miami, USA, and online), speaking on behalf of the Pathfinder I registry investigators. “I think it has really got a lot of traction; we found it a very useful tool across a wide range of plaque morphologies and vessel beds. Further iterations of this platform will hopefully improve its performance further.”
The Auryon atherectomy system (AngioDynamics) “represents an exciting new technology”, John Rundback (Advanced Interventional and Vascular Services, LLP, Teaneck, USA) opined at the International Symposium on Endovascular Therapies (ISET; 9–11 May, Miami, USA, and online), speaking on behalf of the Pathfinder I registry investigators. “I think it has really got a lot of traction; we found it a very useful tool across a wide range of plaque morphologies and vessel beds. Further iterations of this platform will hopefully improve its performance further.”
The Pathfinder registry is a post-market, prospective, multicentre, single arm, all-comers registry of 104 patients with femoropopliteal and tibial stenoses or occlusions or in-stent restenosis (ISR), with peripheral arterial disease (PAD) classified as Rutherford class 2–5. “Lesions of all levels, lesions of all types are included in this real-world registry,” Rundback said.
Patients were treated with either the Auryon atherectomy system or adjuvant therapy. The primary endpoints were acute success (measured as ≤30% final residual stenosis by corelab evaluation) and freedom from peri-procedural major adverse events or complications through 30 days. Long-term results were collected through 24 months, including patency, major adverse events, target lesion revascularisation, and patient-reported outcomes.
Presenting the findings, Rundback said: “These are really important results I think. Across the board, the stenosis reduction or the luminal gain was between 24 and 31%, and this is the laser-cut phenomenon that I think is unique to this laser. In CTOs [chronic total occlusions], there [is an average] 26% luminal gain; [in vessels with] moderate to severe calcium, there was a 27% luminal gain, [in vessels with] ISR, [there was a] 21% luminal gain, and above and below the knee, we see similar levels of luminal gain. So it does not matter what vessel, what vessel calibre, or what the plaque morphology is, this is a very precise, deliverable, controllable, and reproducible result.”
In terms of safety, there was an absence of major adverse events in 99% of lesions. There was one dissection, which was after angioplasty alone, not after laser passage. There were two cases of distal embolization, one of which Rundback said was “probably attributed to the laser”, and one of which was following the treatment of an in-flow lesion that had angioplasty, shockwave, and atherectomy. There were a total of four bailout stents, three of which were for recoil and one of which was for dissection. There was one amputation, which occurred 180 days after follow-up; the patient had Rutherford category 5 disease and gangrene at baseline, and they failed to improve following treatment of their 37cm-long lesion.
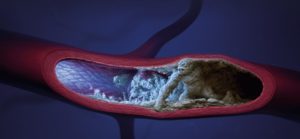
The Auryon atherectomy system is a proprietary, solid-state laser with a wavelength of 355nm (different to the currently-available 308nm laser). “What is really unique about this is it is not just the wavelength, but it has a very short pulse duration of 10ns, which results in a very precise, controllable, and reproducible laser energy delivery to the vessel wall,” Rundback explained.
He went on to describe how this particular wavelength (355nm) has a “very high” affinity for atheroma compared to the vessel endothelium, resulting in a reduced risk of perforation. Indeed, in the Pathfinder I trial, no perforations were reported. There is also less overall thermal damage to the vessel wall, he explained, and the laser system is agnostic to the presence of contrast. It also requires minimal warm-up time: “From a practical point of view, it only needs a 15 second warm-up; if you do not like where it is placed in the room, you can pick it up and move it to another spot.” In addition, Rundback claimed the Auryon atherectomy system is optimal for treating all lesion types.
There are four catheters that are used with this system, ranging from a 0.9mm catheter for below the ankle and in the tibial arteries, to a 2.35mm catheter for the popliteal and superficial femoral arteries. There is also a 2mm catheter for the femoropopliteal and tibioperoneal trunk, and a 1.5mm catheter, for tibial and femoropopliteal arteries.
The Pathfinder registry builds on prior investigational device exemption (IDE) and CE studies, which combined investigated 147 patients with 163 lesions. In these previous research, there were no distal emboli events, and no perforations. Of 107 lesions included in the IDE study, there were just 16 graded as minor dissections (grades A or B). In terms of debulking, there was a 34% reduction post-procedure (the FDA threshold for efficacy is 20%). “Clinical results and patient-reported outcomes were very favourable at 12 months,” Rundback stated.
Session moderator Daniel Clair (Vascular Surgery, University of South Carolina (USC) and the Palmetto Health-USC Medical Group, Columbia, USA) praised Rundback for his talk, saying it offered, “A new look at laser”.