 Suresh Vedantham, professor of Radiology and Surgery, Mallinckrodt Institute of Radiology, Washington University School of Medicine in St Louis, USA, is scheduled to present the final results of the landmark ATTRACT trial on 6 March at the Society of Interventional Radiology’s annual scientific meeting in Washington, DC, USA. The trial’s results will then be discussed by a panel of experts.
Suresh Vedantham, professor of Radiology and Surgery, Mallinckrodt Institute of Radiology, Washington University School of Medicine in St Louis, USA, is scheduled to present the final results of the landmark ATTRACT trial on 6 March at the Society of Interventional Radiology’s annual scientific meeting in Washington, DC, USA. The trial’s results will then be discussed by a panel of experts.
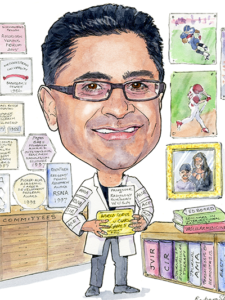
Vedantham is the national principal investigator of the ATTRACT trial and the 2017 incoming president of the SIR. (Get behind the trial data and read his profile in the next issue of Interventional News, available at our booth at the SIR meeting next week).
ATTRACT (Acute venous thrombosis: thrombus removal with adjunctive catheter-directed thrombolysis) set out to determine if the use of pharmacomechanical catheter-directed thrombolysis can prevent the post-thrombotic syndrome in patients with deep vein thrombosis, with acceptable safety and costs.
The trial is a National Institutes of Health-sponsored, phase III, multicentre, randomised, controlled clinical trial. It is a major international collaborative effort among leading North American researchers of diverse subspecialty.
“[At the time this publication goes to print] I am not yet free to discuss the trial’s findings, but I do believe this trial achieved its main objective of telling us which acute deep vein thrombosis patients should, or should not, receive endovascular intervention,” Vedantham, professor of Radiology and Surgery, Mallinckrodt Institute of Radiology, Washington University School of Medicine, St Louis, USA, and the 2017 incoming president-elect of the Society of Interventional Radiology (SIR) told Interventional News ahead of the presentation.
Here is a teaser (and a few outtakes from the interview), available exclusively on our website.
Could you comment on the importance of multidisciplinary collaboration and its value in the running of large-scale clinical trials such as the ATTRACT trial?
First, interacting with other providers enables one to understand the disease in a broader context that goes beyond one procedure or category of intervention. It pushes you to challenge your own groupthink. We tend to forget that our view on a disease is shaped by many factors: the clinical setting in which we see patients; the mindset of our colleagues; and (both for better and for worse) the effect of industry (the drug industry for internists and the device industry for endovascular physicians) upon all of it. Training matters too—internists view deep venous thrombosis as basically an imbalance in the clotting system; whereas we view it from anatomical and physiological perspectives. Only when we share these camera angles with each other can we see a fuller picture.
Second, collaborating recruits skills that one would not have otherwise. What I have learned from ATTRACT is pretty humbling. Despite being considered a “research leader”, the truth of the matter is that I am first and foremost a well-trained clinician who does research on the side. But many of the other leaders in the ATTRACT trial are professionally trained researchers, and believe me it shows. The trial could never have been designed, funded, and completed without all kinds of different expertise being brought to bear on it.
Third, your potential to have real clinical impact, and stave off challenges to your study, is multiplied manyfold by collaborating. My best advice to young researchers would be that you need to be able to speak the language of multiple subspecialties around the condition you are studying. That means knowing their literature, guidelines, and culture. Only when they see that you appreciate their perspectives can they reach beyond them to understand yours. And, do not be put off by bumps in the road; they are inevitable. The amazing thing I have seen with ATTRACT is that over 10 years, our steering committee members have actually grown together in their individual perspectives on deep venous thrombosis, learning from each other along the way.
As a member of various writing groups on the treatment of venous thromboembolism, what are the most important changes in the latest guidelines?
Recently developed guidelines include updated quality improvement guidelines for interventions from SIR (2014); the first guideline to focus on the diagnosis, prevention, and management of post-thrombotic syndrome from the American Heart Association (AHA, 2014); the Anticoagulation Forum’s practice-oriented chapters on venous thromboembolism management (2016); and of course, the 2016 Chest Guidelines update. Important changes include recommendations supporting the use of new oral anticoagulants for venous thromboembolism care, the weakening of recommendations for compression stockings in acute deep venous thrombosis patients (due to the results of the rigorous SOX trial which were negative), slightly more attention to chronic sequelae of venous thromboembolism including post-thrombotic syndrome, and the continued need for clinical trial evidence to guide recommendations on endovascular care options.
From your 2007 paper “Myths, misconceptions, and incorrect interpretations of the deep venous thrombosis literature”, which of these hold true ten years later?
I would say it continues to be important to consider deep venous thrombosis and post-thrombotic syndrome as “diseases” with multifactorial aetiologies. It continues to be important to ensure quality anticoagulation for deep venous thrombosis. One thing that has changed since 2007 is that compression therapy has been found in a recent rigorous, double-blind, multicentre randomised trial not to prevent post-thrombotic syndrome. It continues to be important not to draw outsized inferences from observational associations and data from low-quality studies. We need to keep pushing the envelope by completing multiple highly rigorous studies to drive us forward.
Stay tuned for more…













